Copy link
Axillary Block
Last updated: 04/20/2023
Key Points
- The axillary block is a valuable block for surgeries of the elbow, forearm, wrist, and hand.
- Identifying relevant anatomical landmarks will aid in successful procedural outcomes.
- The axillary block is a low-risk procedure. However, vessels are easily compressible in this location, which may conceal the presence of vascular structures. Caution should be taken to avoid inadvertent intravascular injection.
- Light probe pressure, frequent aspiration, slow injection of the local anesthetic, and appropriate local anesthetic spread under ultrasound guidance can all help to reduce this risk.
Indications
- The axillary block is useful as a preoperative block for surgeries of the elbow, forearm, wrist, and hand.1-3
- The aim is to anesthetize four of the five terminal branches of the brachial plexus: the median, radial, ulnar, and musculocutaneous nerves.
- Notably, the musculocutaneous nerve departs from the lateral cord in the proximal axilla. It lies lateral to the axillary artery and will be spared unless a separate injection is performed.
- The medial antebrachial nerve, although not specifically targeted, often follows the median nerve within the neurovascular sheath and is invariably blocked.
- Together, these nerves provide complete coverage distal to the elbow.
- Nerves that are spared while performing an axillary block include:
- axillary (sensory to the shoulder joint and lateral arm, motor to the deltoid and teres minor muscles);
- medial brachial cutaneous (sensory to the medial aspect of the arm as far distal as the medial epicondyle of the humerus and olecranon of the ulna);
- intercostobrachial nerves (sensory to the lateral chest, axilla, and medial aspect of the arm); and
- given the unreliable blockade of these nerves, the axillary block does not provide adequate coverage proximal to the elbow.1
Anatomy and Clinical Correlates
Landmarks and Surrounding Structures
- The most pragmatic landmark to identify prior to performing an axillary block is the axillary artery. The axillary artery’s easy visibility serves as the “centerpiece” of which the median, radial and ulnar nerves surround.
- The median, radial, and ulnar nerves are branches of the brachial plexus, which originate from C5-T1. These nerves may be targeted at varying levels of the brachial plexus, resulting in different cutaneous innervation patterns.
- The conjoint tendon of the latissimus dorsi and teres major is another key landmark. Visibility of this tendon ensures that all nerves, apart from the musculocutaneous nerve, will be located around the artery above the tendon.
- Though there can be anatomic variability at the axillary level, the corresponding nerves may be identified relative to the axillary artery in a clock-face orientation with the arm in 90° abduction (Figure 1).4
- Median nerve (anterior and lateral to the axillary artery): 10-12 o’clock position
- Radial nerve (posterior to the axillary artery): 6-8 o’clock position
- Ulnar nerve (anterior and medial to the axillary artery): 1-4 o’clock position
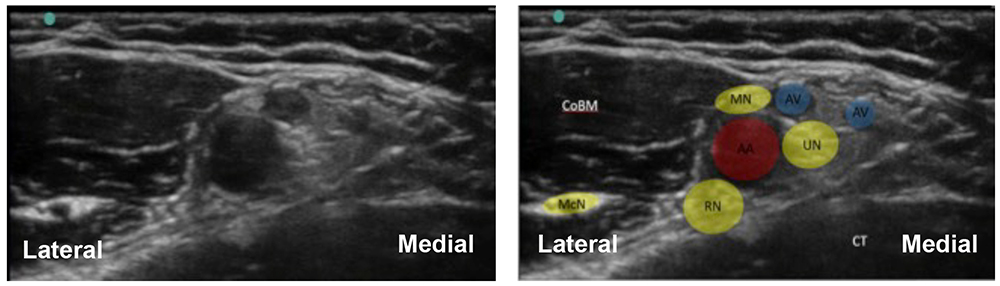
Figure 1. Ultrasonography of axillary nerve block. AA = axillary artery, AV = axillary vein, McN = musculocutaneous nerve, RN = radial nerve, UN = ulnar nerve, MN = median nerve, CoBM = coracobrachialis muscle, CT = conjoint tendon. Source: Wingate R, Foxall G. Ultrasound-guided axillary brachial plexus block. World Federation of Societies of Anaesthesiologists. CC BY NC ND 4.0. Link.
Cutaneous Innervation
- The five main terminal branches of the brachial plexus (axillary, musculocutaneous, median, ulnar and radial) are formed from the three cords of the brachial plexus (lateral, medial, and posterior) in the apex of the axilla. The median, ulnar and radial nerves are encased in an axillary sheath and surround the axillary artery, while the axillary and musculocutaneous nerves leave the plexus at the level of the coracoid process.
Median Nerve
- The median nerve is a terminal branch of the lateral and medial cords (C6-T1).
- Sensory innervation: lateral aspect of the palmar surface of the hand, palmar surface of the 1st-3rd digits and lateral half of the 4th digit, along with the dorsal aspect past the proximal interphalangeal joint (over the nail beds).
- Motor innervation: flexor muscles of the forearm and hand, including muscles responsible for flexion, abduction, opposition, and extension of the thumb.
Radial Nerve
- The radial nerve is a terminal branch of the posterior cord (C5-T1).
- Sensory innervation: lateral aspect of the distal arm inferior to the insertion of the deltoid muscle, posterior aspect of the arm, and a strip down the middle of the posterior forearm. The superficial branch is a terminal division and innervates the dorsal surface of the hand, including the lateral three and a half digits.
- Motor innervation: extensor muscles of the arm, forearm, and hand.
Ulnar Nerve
- The ulnar nerve is a terminal branch of the medial cord (C8-T1).
- Sensory innervation: medial elbow, forearm, and ulnar aspect of the palmar surface of the hand. It also provides sensation to the 5th digit and the ulnar half of the 4th digit.
- Motor innervation: extensor muscles of the arm, forearm, and hand.
Musculocutaneous Nerve
- The musculocutaneous nerve is a terminal branch of the lateral cord (C5-C7). It departs in the proximal axilla to lie within the fascial plane between the biceps brachii and coracobrachialis muscle or within the belly of the coracobrachialis muscle. As it enters the forearm it continues as the lateral cutaneous nerve of the forearm, also known as the lateral antebrachial cutaneous nerve.
- Sensory innervation: lateral aspect of the forearm
- Motor innervation: muscles of the anterior compartment of the arm: coracobrachialis, biceps brachii, and brachialis muscles
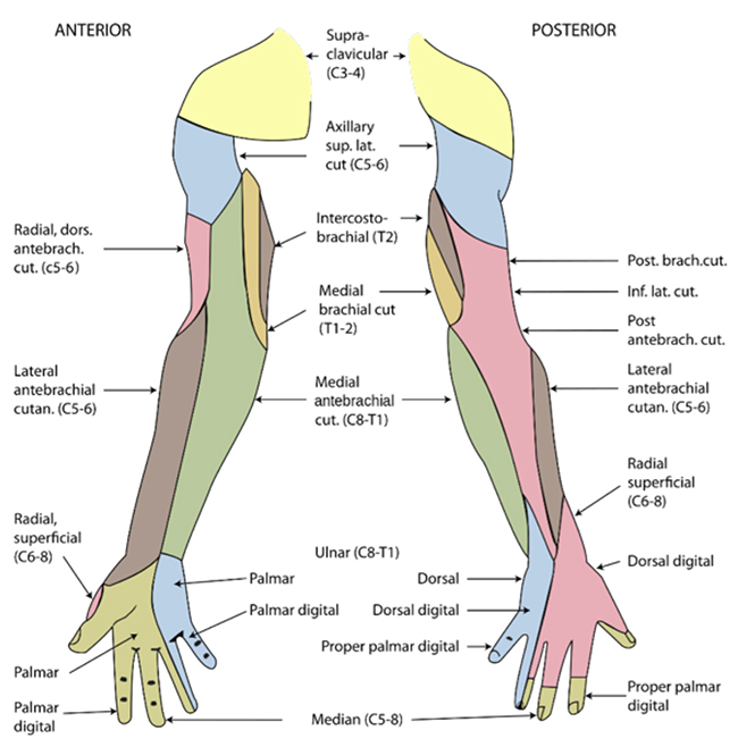
Figure 2. Sensory innervation of the upper limb. Source: Wikimedia Commons. Henry Vandyke Carter, Public domain. Link.
Contraindications
Absolute: Patient refusal, infection at the injection site, malignancy at the site of injection
Relative: Preexisting neurological disease including paresis or paresthesias, severe coagulopathy
Equipment and Materials
- Ultrasound with linear transducer (8-14 mHz), sterile sleeve and gel
- Sterile gloves
- 3-5 mL syringe with 1.5 inch, 25-gauge needle (for local anesthesia of the skin)
- 1-2x 20 mL syringes
- 50mm 22-gauge echogenic needle
- If using nerve stimulation, a peripheral nerve stimulator and stimulating needle should also be included.
- Medication options:
- Short-acting: 1-2% lidocaine
- Long-acting: 0.25-0.5% bupivacaine or 0.2-0.5% ropivacaine
- Epinephrine 2.5 mcg/mL is recommended as a marker for inadvertent intravascular injection.5
Positioning
- The patient should be placed in a supine position with the arm abducted to 90° with the elbow flexed and the shoulder externally rotated (Figure 3).
- A high-frequency probe is placed in a transverse orientation over the axillary artery against the pectoral fold. The ultrasound depth may be initially set at 3-3.5cm.

Figure 3. Needle insertion site (circle on the skin) and probe position during image acquisition. Used with permission from Remerand F, et al. Is the musculocutaneous nerve really in the coracobrachialis muscle when performing an axillary block? An ultrasound study. Anesth Analg. 2010.6
Techniques
- When performing an ultrasound-guided axillary block, two techniques are possible: perineural or perivascular.
- The perineural technique targets each of the specific nerves individually.
- The perivascular technique aims to achieve a circumferential spread around the axillary artery, essentially bathing the nerves in the injectate within the neurovascular sheath. The perivascular technique can be beneficial if the individual nerves are not easily identifiable.
- Both techniques are effective in achieving a suitable block. However, the perivascular technique will shorten the overall procedure time but may delay the onset of anesthesia.1,7
Steps
- After the skin is disinfected, a sterile covered transducer is placed in a short-axis orientation to the axillary artery in the axilla.
- A preprocedural scan should be performed by identifying landmarks/targets, and ensuring visualization of anatomy, any anatomical variants or pathology. Specifically, the axillary artery should be located with the three primary surrounding targets of the median, radial, and ulnar nerves (Figure 4) and the conjoint tendon below.
- One to 2 mL of 1% lidocaine should be injected using a 25g needle for skin analgesia. The needle is directed in-plane from the anterior to posterior direction.
- For a perineural approach: An echogenic block needle in-plane should be inserted, from anterior to posterior, with a trajectory toward the radial nerve, posterior to the axillary artery. Injections should be performed as follows:
- Radial nerve: aim the needle tip between the radial nerve and the axillary artery above the conjoint tendon. Inject 5-10 mL of injectate.
- Ulnar nerve: partially withdraw the needle and direct the needle tip superiorly over the axillary artery (while circumventing the median nerve) adjacent to the ulnar nerve. Inject 5-10 mL of injectate between the axillary artery and ulnar nerve.
- Median nerve: partially withdraw the needle, so the tip is to position the tip placed next to the median nerve. Inject 5-10 mL of injectate.
- Musculocutaneous nerve: position the needle tip, so it rests adjacent to the nerve. Inject 3-5 mL of injectate.
- For a perivascular approach: Proceed with Step #4a. Inject 10 mL of the local anesthetic just posterior to the axillary artery. Inject another 10 mL of the local anesthetic just anterior to the artery, ensuring a complete circumferential spread of the hypoechoic injectate evident on ultrasound. Step #4d may need to be performed to anesthetize the musculocutaneous nerve. Total injectate is 20-30 mL.
- If desired, a continuous block with catheter placement can be performed.
- The needle is inserted as above (anterior to posterior), with the tip placed next to the nerve most relevant to the surgery.
- A catheter can then be threaded 3-5 cm past the needle tip.
- Care must be taken given the vascularity at this site.
- If desired, a continuous block with catheter placement can be performed.
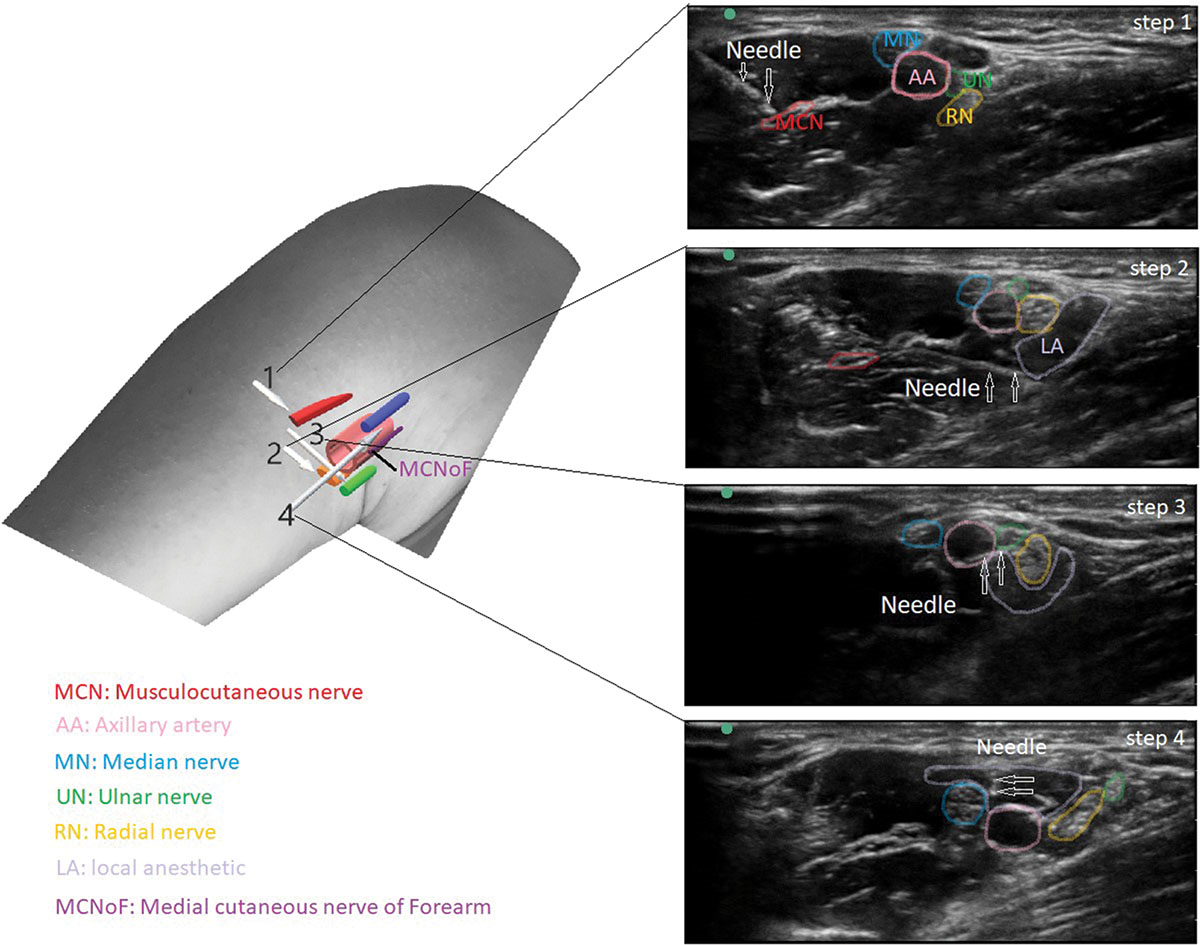
Figure 4. Arrows show the needle course to the tip of the needle. AA, axillary artery; LA, local anesthetic; MCN, musculocutaneous nerve; MCNoF, medial cutaneous nerve of forearm; MN, median nerve; RN, radial nerve; UN, ulnar nerve. Used with permission from Garnaud T, et al. Novel axillary block management for tendon transfer surgery: A case report. A A Pract. 2019.8
Caution and Complications
- The axillary block is typically very low risk with few reported complications.
- The primary area of caution, however, is to ensure avoidance of intravascular injection due to the superficial nature of the vessels and ease of compressibility.
- Infection and hematoma risks are possible but extremely rare.
- Nerve damage of the brachial plexus or terminal branches (median, radial, and ulnar nerves) is a rare complication.
- This can be prevented with the use of ultrasound guidance, good visualization of the needle, low injection pressures, and proper spread of medication.
References
- Ranganath A, Srinivasan KK, Iohom G: Ultrasound-guided axillary brachial plexus block. Med Ultrason. 2014;16: 246–51. PubMed
- Retzl G, Kapral S, Greher M, et al. Ultrasonographic findings of the axillary part of the brachial plexus. Anesth Analg. 2001; 92:1271-5. PubMed
- Chin KJ, Cubillos JE, Alakkad H. Single, double or multiple-injection techniques for non-ultrasound guided axillary brachial plexus block in adults undergoing surgery of the lower arm. Cochrane Database Syst Rev. 2016; 9:CD003842. PubMed
- Christophe JL, Berthier F, Boillot A, et al. Assessment of topographic brachial plexus nerves variations at the axilla using ultrasonography. Br J Anaesth. 2009;103(4):606-12. PubMed
- Dolan J, McKinlay S. Early detection of intravascular injection during ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2009; 34:182. PubMed
- Remerand F, Laulan J, Couvret C, et al. Is the musculocutaneous nerve really in the coracobrachialis muscle when performing an axillary block? An ultrasound study. Anesth Analg. 2010. 110(6): 1729-34. PubMed
- Bernucci F, Gonzalez AP, Finlayson RJ, et al. A prospective, randomized comparison between perivascular and perineural ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012; 37:473-7. PubMed
- Garnaud T, Toulemonde J. Novel axillary block management for tendon transfer surgery: A case report. A A Pract. 2019. 12(12): 426-9. PubMed
Other References
- Wingate R, Foxall G. Ultrasound-guided axillary brachial plexus block. Anesthesia Tutorial of the Week 326. World Federation of Societies of Anaesthesiologists. Accessed March 6th, 2023. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.