Copy link
ABCs of Blood Transfusions
Last updated: 03/02/2023
Key Points
- The transfusion of ABO-incompatible blood is considered a “never event.”
- Careful ABO and Rh typing, antibody screening, and blood crossmatching form the backbone of pretransfusion testing to ensure donor and recipient compatibility.
- Blood products must have appropriate additives and be stored at appropriate temperatures to ensure their longevity and viability.
Introduction
- Safe handling and administration of blood products represent a critical component of the practice of anesthesiology, and concepts of transfusion medicine are included in the board certification process for anesthesiologists.1
- Anesthesiologists order over 50% of all blood products in large hospitals and work in settings where just under half of all blood products are administered.1
- A methodical approach to typing, screening, crossmatching, and administering blood products can ensure patients receive necessary transfusions in a safe and timely manner.
ABO Blood Types
- There are four main blood types: A, B, AB, and O. A person’s blood type is defined by whether or not the A and/or B antigens are expressed on their red blood cells (RBCs).2
- A person naturally develops antibodies to the A and B antigens if they are not expressed on their own RBCs after approximately 3 months of life.2
- Antibodies to A and B are mostly made up of IgM immunoglobulins and will develop visible agglutination when mixed with RBCs with antigens they are targeted against. For example, a person with blood type A will have naturally occurring anti-B antibodies that will agglutinate when exposed to type B or type AB RBCs (Table 1).
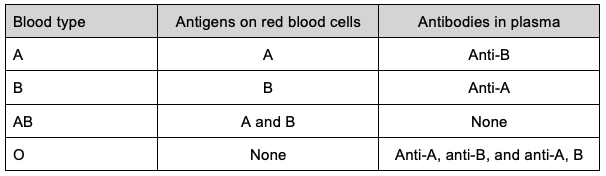
Table 1. ABO blood types and corresponding antigens and antibodies.
- The transfusion of ABO-incompatible blood can lead to an acute hemolytic transfusion reaction by activating the complement pathway leading to intravascular hemolysis and the release of cytokines that can lead to disseminated intravascular coagulation, shock, and death. Transfusion of as little as 10mL of ABO-incompatible blood can lead to an acute hemolytic transfusion reaction.2
- Transfusion of ABO-incompatible blood is considered a never event in nearly all health care systems.2
RhD Antigen
- Besides the ABO antigens, RBCs also express other minor red cell antigens. Their clinical significance varies, with the most clinically significant antigens belonging to the Rh blood group. Of the Rh antigens, the most clinically important is RhD.2
- A person whose RBCs express the D antigen is said to be RhD positive, whereas a person whose RBCs do not express the D antigen is said to be RhD negative. In addition, D variants exist, such as partial D and weak D, in which there can be quantitative and qualitative differences in an individual’s expression of the D antigen.3
- Different populations have different frequencies of expression of the D antigen on RBCs.
- Antibodies to D are typically only developed in RhD negative people exposed to D-positive blood, either through transfusion of D-positive blood or through pregnancy with D-positive fetuses. In other words, anti-D alloantibodies are not naturally occurring and require a sensitizing event. Because RhD negative people lack the D antigen, they are at risk of making anti-D antibodies if exposed to the antigen.
- Transfusing D-positive blood to an individual with anti-D antibodies can lead to a hemolytic transfusion reaction. Anti-D antibodies also have the potential to cause hemolytic disease of the fetus and newborn.2
- Typically, RhD positive individuals can safely receive either D-positive or D-negative RBCs. RhD negative individuals typically only receive D-negative RBCs to prevent anti-D antibody formation, except in emergencies or in times of D-negative blood shortages. RhD negative individuals who already have anti-D antibodies should only receive D-negative RBCs.
- Whenever possible, it is important to avoid transfusing RhD negative females of childbearing potential D-positive blood, as this may complicate future pregnancies.
Type and Screen
- A type and screen is a component of pretransfusion testing in which the blood of a potential transfusion recipient is evaluated to determine ABO type and RhD type and evaluate for the presence of antibodies directed against red blood cell antigens.4
- Type and screens should be performed when there is a potential transfusion need identified in a patient. Once a type and screen has been performed, compatible blood can be identified and issued to the patient as long as the type and screen is valid. An order for a type and screen, compared to an order for a type and cross, does not typically reserve specific units for a patient.4
- Type and screens may only be valid for certain time frames. For example, a type and screen is valid for three days for an adult patient who has been recently transfused or pregnant within the last three months. Once the type and screen “expires,” a new type and screen must be ordered and performed if the patient requires further transfusion in order to ensure the patient receives compatible units.
ABO and Rh Type
- Determination of an accurate ABO and RhD type for all donors and recipients is critically important to avoid the catastrophic consequences of transfusion of incompatible blood.3
- To determine the ABO blood type, both a forward type and reverse type are performed (except in neonates who are only tested with forward typing). Forward typing uses reagent anti-A and anti-B antisera to determine if the A and/or B antigens are expressed on the patient’s red cells, and backward typing tests patient plasma against reagent A and B RBCs to determine if the patient has anti-A and/or anti-B antibodies. Performing forward and reverse types and looking for discrepancies helps confirm an accurate ABO type.4
- RhD typing is performed using reagent anti-D antisera to determine if the patient’s RBCs express the D antigen.
Antibody Screen
- Antibody screens are performed to identify if an individual has antibodies directed against other RBC antigens besides ABO.4
- A potential transfusion recipient’s serum is mixed with reagent RBCs that are known to express certain RBC antigens. The reagent RBCs are type O to avoid reaction with anti-A and anti-B antibodies that may be present in a recipient’s serum.4
- After mixing a recipient’s serum with reagent RBCs, anti-human globulin (AHG) is added (an indirect antiglobulin test) which will result in agglutination if IgG antibodies directed against RBCs are present in the recipient’s serum.4
- If agglutination occurs, the antibody screen is positive and further testing must be performed to identify what antigen a recipient has antibodies against.4
- The antibody screen and subsequent antibody identification can identify both autoantibodies and alloantibodies. Not all RBC antibodies are considered clinically significant. If a patient has RBC antibodies, additional phenotypic requirements besides ABO and RhD compatibility may be required, which can lead to delays in finding and issuing compatible blood.
Type and Cross
- A type and cross is an order for pretransfusion compatibility testing that includes a type and screen but adds an additional step, the crossmatch, in order to find crossmatch compatible blood. The crossmatch determines if the recipient’s plasma is compatible with a specific donor unit. This can be done in multiple ways. If the unit(s) is compatible, this blood is typically held and reserved for this patient for a specified time.4
- For a recipient who has a negative antibody screen, no previous history of RBC antibodies, and an ABO type performed on two separate occasions, a crossmatch can be performed electronically or using an immediate spin method.5
- In an electronic crossmatch, a validated computer algorithm ensures that the recipient’s two separate ABO types match and then identifies a compatible donor unit.5
- In facilities without electronic crossmatching capabilities, an immediate spin method can be used instead on patients who meet the same above criteria. The immediate spin crossmatch involves mixing recipient plasma with a donor unit and evaluating for hemolysis or agglutination. If no hemolysis or agglutination is observed (a negative crossmatch), the unit is compatible and can be released to the patient.4
- Both the electronic and immediate spin crossmatch take only a few minutes to perform.
- In situations where the antibody screen is positive, a patient has a history of a clinically significant antibody, or if the immediate spin crossmatch results in agglutination or hemolysis (a positive crossmatch), a full IgG crossmatch is performed.4
- A full IgG crossmatch involves mixing recipient plasma with donor RBCs and performing an indirect antiglobulin test. This process and finding compatible blood can take several hours or more depending on a patient’s serologic complexity.4
Properties of Stored Blood
- Several changes occur in stored blood over time. Collectively, the changes are referred to as storage lesions, and they include:
- Increase in potassium secondary to hemolysis
- Oxidative damage to RBCs leading to increased free hemoglobin and reactive oxygen species
- Lactate and cytokine accumulation
- Rapid decline in 2,3-diphosphoglycerate (2,3-DPG) levels, which affects the ability of hemoglobin to release bound oxygen. However, once in circulation, stored RBCs regenerate 2,3-DPG within 72 hours.6
- The storage temperature and shelf life of blood products are listed in Table 2.
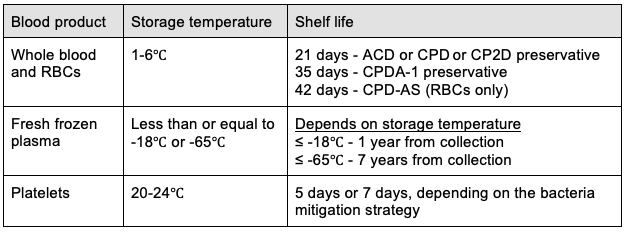
Table 2. Blood Product Storage Shelf Lives6,7 Abbreviations: ACD = Acid citrate dextrose; CPD = Citrate phosphate dextrose; CPDA-1 - Citrate phosphate dextrose adenine; CPD-AS = Citrate phosphate dextrose with additive solution AS-1, AS-3, or AS-5.
RBC Additives
- Anticoagulant solutions are added to whole blood during collection to prevent clotting and provide nutrients to RBCs to maintain their viability. Additives contain sodium citrate, dextrose, and citric acid, with the possible addition of phosphate and adenine.6
- RBC units prepared from whole blood require both suspension in an adequate fluid volume to allow for sufficient flow during transfusion and the addition of nutrients for cell survival and viability.6
- Dextrose and adenine are most commonly added to RBCs to provide an adequate nutrient source.
- The volume of additive solution required to preserve stored RBCs varies relative to the volume of whole blood the RBCs are prepared from, with larger volumes of whole blood requiring large volumes of additive solution.6
References
- Aldarweesh F, Rose WN. Transfusion medicine education for anesthesiology residents: A novel curriculum. Acad Pathol. 2019; 6:2374289519855729. PubMed
- Norfolk D, ed. Handbook of Transfusion Medicine. Fifth Edition. Sheffield: The Stationary Office (TSO); 2013.
- Dudley M, Miller R, Turnbull J. Patient Blood Management: Transfusion Therapy. In: Gropper M, ed. Miller’s Anesthesia. Ninth Edition. Philadelphia, PA: Elsevier; 2020:1546-78.
- Armstrong B, Wilkinson R, Smart E, et al. Compatibility testing. ISBT Sci Ser. 2020;15(S1):255-276. Link
- Chapman JF, Milkins C, Voak D. The computer crossmatch: a safe alternative to the serological crossmatch. Transfus Med. 2000;10(4):251-6. PubMed
- Hardwick J, reviewer for second edition: Al-Riyami A. Blood storage and transportation. ISBT Sci Ser. 2020;15(S1):232-54. Link
- Standards for Blood Banks and Transfusion Services. 33rd ed. Association for the Advancement of Blood and Biotherapies. 2022.
Other References
- Mark N. Blood Product Transfusions. ICU One Pagers. Accessed February 22, 2023. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.