Copy link
Celiac Plexus Block
Last updated: 02/12/2024
Key Points
- The celiac plexus is a key target point of pain transmission from the upper abdominal organs, and therefore, neurolysis is an effective method of controlling pain from these organs.
- Primary indications for performing a celiac plexus block (CPB) include intractable abdominal pain secondary to upper abdominal malignancies, most notably pancreatic cancer.
- The most common adverse effects from CPB include orthostatic hypotension and diarrhea, though these are usually transient and self-limiting.
Introduction
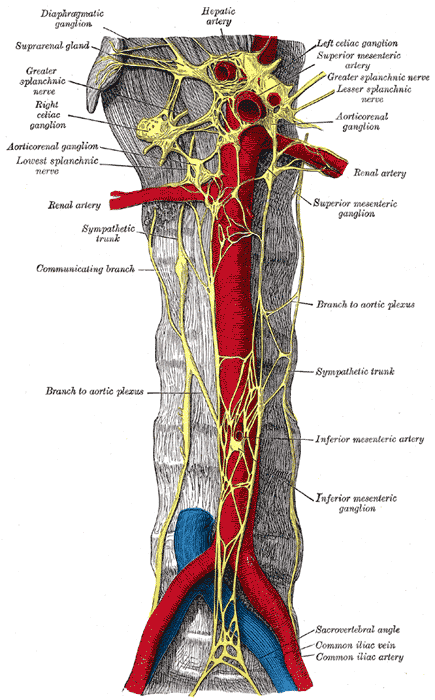
- The celiac plexus, also known as the solar plexus, is the largest autonomic plexus and is a network of paired celiac ganglia and smaller ganglia, including the superior mesenteric ganglia and aorticorenal ganglia (Figure 1).1,2
- The celiac plexus is located deep in the retroperitoneal fat over the anterolateral surface of the aorta, epigastrium, crus of the diaphragm, and posterior to the stomach and pancreas.
- The most common locations of the plexus are at the levels of T11/12 (6.5%), T12 (34%), T12/L1(31%), and L1(28.5%).2 The mean size of the ganglia is about 2.7 cm, and the left ganglion is slightly below the right ganglion.
- The celiac plexus is primarily composed of efferent preganglionic sympathetic fibers from the greater (T5-T10), lesser (T10-T11), and least (T12) splanchnic nerves, and preganglionic parasympathetic fibers from the vagus nerves. Afferent nociceptive fibers from the upper abdominal organs (stomach to midtransverse colon, pancreas, gall bladder) pass through the celiac plexus and accompany the sympathetic fibers.
- The celiac plexus is a key target point of pain transmission from the upper abdominal organs, and therefore, neurolysis is an effective method of controlling pain from these organs.3
Indications
- The primary indication for celiac plexus block (CPB), also known as celiac plexus neurolysis, is intractable abdominovisceral pain refractory to standard analgesic interventions.1-3 This effective procedure is frequently used in upper abdominal malignancies, most notably inoperable pancreatic cancer. Other cancers for which CPB is utilized include:
- Stomach cancer
- Esophageal cancer
- Colorectal cancer
- Liver cancer
- Gallbladder cancer
- Bile duct cancer
- Noncancerous conditions in which CPB is utilized include:
- Chronic pancreatitis
- Diabetic gastroparesis
- CPB is often recommended if a patient fails one to two trials of opioid therapy or prefers a nonpharmacologic approach.4 A significant advantage of this procedure is the potential for reducing opioid consumption and opioid-related side effects and complications.2
Techniques
- Several techniques have been described to block the celiac plexus, including posterior paraaortic, anterior paraaortic, posterior transaortic, transintervertebral disc, and endoscopic approaches (Figure 2).
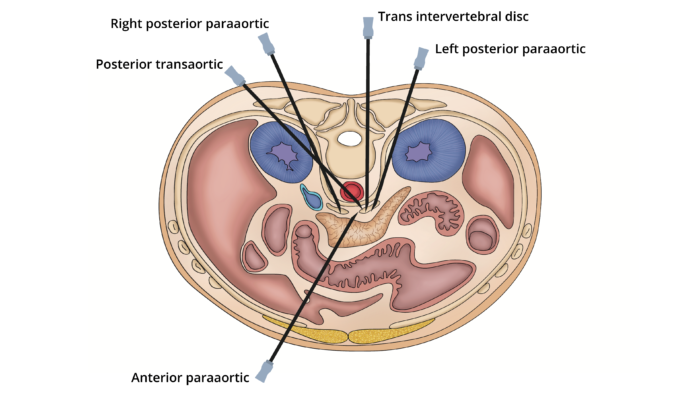
Figure 2. Different approaches to perform the CPB. Adapted from Urits I, et al. A comprehensive review of the celiac plexus block for the management of chronic abdominal pain. Cur Pain Headache Rep. 2020; 24(8): 42. PubMed
- Increasingly, these blocks are being performed under computed tomography, ultrasonographic, fluoroscopy, or magnetic resonance imaging guidance with improved success rates and fewer complications.2.3
- A thorough workup should be completed prior to the procedure to exclude contraindications such as severe coagulopathy, thrombocytopenia, abdominal aortic aneurysm, eccentric origin of the celiac artery, inability to visualize local anatomy due to large overlying soft tissue mass, etc.4
Posterior Paraaortic Approach
- This is the most commonly used approach. Patient positioning is either prone or lateral decubitus. After preprocedure imaging and selecting a safe path to the celiac plexus, a 20-22G needle is advanced to position the needle tip 1-2 cm anterior and lateral to the aorta between the levels of the superior mesenteric artery and celiac trunk. Once proper placement has been confirmed, 20-30 mL of 50-100% ethanol or 20-25 mL of 3-20% phenol is slowly injected on either side of the aorta.
Anterior Paraaortic Approach
- This approach requires traversing through the visceral organs, and intraprocedural imaging is usually used to guide the needle path.
- It is usually reserved for terminally ill patients who are unable to tolerate prone positioning or patients with altered anatomy or tumor invasion preventing posterior access.
Posterior Transaortic Approach
- After the patient is in the prone position, the needle is inserted at the level of the first lumbar vertebrae and advanced along a left paravertebral trajectory. The needle is then advanced through the posterior and anterior walls of the aorta to reach the preaortic space. Correct placement is confirmed by negative aspiration and injection of contrast material.
Transintervertebral Disc Approach
- In this approach, the needle is inserted through the T12-L1 or L1-L2 intervertebral disc to reach the intercrural space anterolateral to the aorta.
Endoscopic Ultrasound-Guided (EUS) Approach
- In this approach, a curvilinear array echoendoscope is inserted through the mouth and advanced to the posterior lesser curve of the fundus of the stomach to identify the aorta. The needle is inserted through the biopsy channel of the endoscope, and then, under ultrasound guidance, the needle is inserted through the gastric wall into the celiac region.5
Neurolysis vs. Blocking Agents
- Neurolytic agents, such as ethanol and phenol, are used when the CPB is performed for cancer pain. Phenol is historically the medication of choice as it is less irritating and more tolerated than ethanol. However, recently, ethanol is used more commonly than phenol because it is more readily available. Steroid injections, such as dexamethasone are used when the CPB is performed to decrease edema and inflammation in conditions such as chronic pancreatitis.3
- Local anesthetics (bupivacaine or lidocaine) are used with steroids and ethanol to counteract the pain during injection. On the other hand, phenol has anesthetic effects and does not require the addition of a local anesthetic.3
- Typically, 30-50 mL of ethanol is injected into the intercrural space, and 15-30 mL is injected into the retrocrural space. Ethanol concentrations vary from 50-100%.3
- Typically, 15-25 mL of phenol is injected into the intercrural space, and 3-10 mL is injected into the retrocrural space. Phenol concentrations vary from 3-20%.3
Adverse Effects and Complications
- The most common complaint following a CPB is transient back pain at the site of the injection.3,4
- Orthostatic hypotension and diarrhea are the most common side effects following a successful block.2-4 Hypotension is caused by the loss of sympathetic tone of the splanchnic vessels, resulting in vasodilation. Therefore, the patient should receive a fluid bolus prior to the block. Diarrhea occurs due to sympathetic blockade and unopposed parasympathetic efferent influence.
- Accidental intravascular injection into the vena cava or aorta can cause serious reactions.
- Other less common complications include:2-4
- Retroperitoneal hematoma
- Injury to surrounding structures (kidney or pancreas)
- Pneumothorax
- Chylothorax
- Bleeding
- Sexual dysfunction
- Paraplegia (due to spasm of or injury to the artery of Adamkiewicz)
References
- John RS, Dixon B, Shienbaum R. Celiac plexus block. In: StatPearls (Internet). Treasure Island, FL, StatPearls Publishing. 2023. Link
- Rana MV, Candido KD, Raja O, et al. Celiac plexus block in the management of chronic abdominal pain. Curr Pain Headache Rep. 2014;18(2):394. PubMed
- Urits I, Jones MR, Orhurhu V, et al. A comprehensive review of the celiac plexus block for the management of chronic abdominal pain. Cur Pain Headache Rep. 2020; 24(8): 42. PubMed
- Gunduz OH, Kenis-Coskun O. Ganglion blocks as a treatment of pain: Current perspectives. J Pain Res. 2017; 10:2815–26. PubMed
- Wiersema MJ, Saumoy M. Endoscopic ultrasound-guided celiac plexus interventions for pain related to pancreatic disease. In: Post T, ed. UpToDate; 2023. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.