Copy link
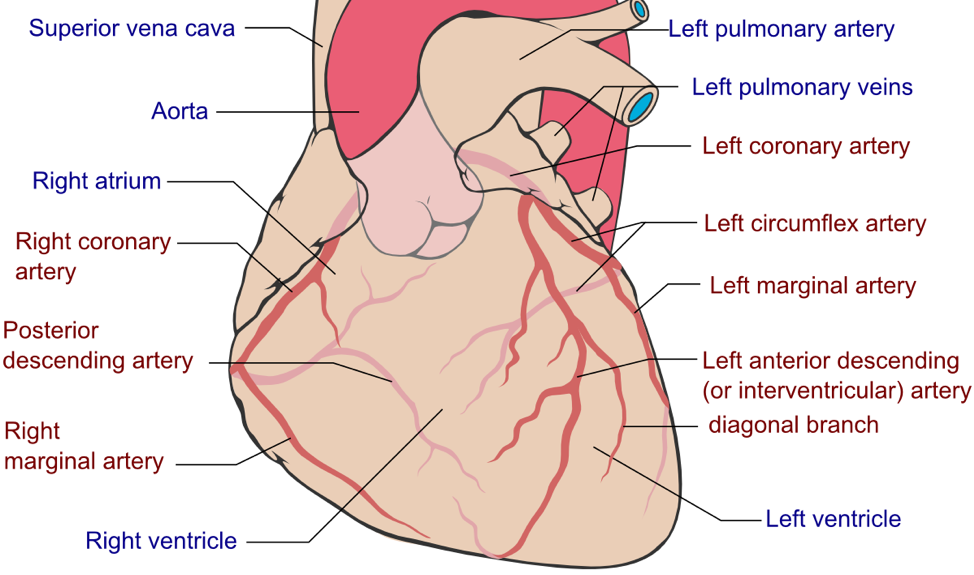
Coronary artery distribution
Last updated: 06/06/2018
Coronary Dominance: Dominance is determined by the coronary artery that crosses the junction between atria and ventricles to supply the posterior descending coronary branch. Though various estimates exist, Barash’s Clinical Anesthesia approximates that 50% of humans are right coronary artery dominant. The other 50% are either co-dominant (30%) or left coronary artery dominant (20%).
Coronary Origin: The two coronary arteries, left and right, originate from the left and right sinuses of Valsalva within the aortic valve. The sinuses of Valsalva provide space behind the open aortic leaflets that prohibit leaflet occlusion of the coronary artery orifices.
Left Coronary Artery: The left coronary artery (LCA) emerges between the body of the left atrium and the pulmonary artery, curving anteriorly about the latter vessel towards the anterior interventricular sulcus. After a short course, the LCA bifurcates into the left anterior descending artery (LAD) and the circumflex artery (CX). The LAD courses downward over the anterior left ventricular wall, providing diagonal and septal perforator branches along its course. The CX follows the atrioventricular groove, giving off the left marginal artery. In left coronary dominant humans, the posterior descending artery emerges from the CX.
The LCA and its branches generally supply the left atrium, the interventricular septum, and the anterolateral left ventricle. They partially supply the posterior left ventricular wall, the right and left bundle branches, and the anterior and posterior papillary muscles of the mitral valve. LAD occlusion produces ischemic changes in ECG leads V3 through V5, while CX occlusion produces changes in ECG leads I and aVL.
Right Coronary Artery: The right coronary artery (RCA) lies near the middle of the right coronary sinus of Valsalva. In about 50% of people, the RCA immediately gives off the conus artery, which provides a potentially important source of collateral circulation in the event of LAD occlusion. The sinus node and AV nodal arteries emerge shortly thereafter. In the 80% of humans with right-dominant circulation, the RCA gives off the posterior descending artery (PDA), which passes between the body of the right atrium and the main pulmonary artery into the right atrioventricular sulcus. The RCA also gives off the right marginal artery, which descends toward the apex, terminating as several parallel trunks descending in or near the posterior interventricular sulcus toward the terminal branches of the LAD.
The RCA and its branches usually supply both the SA and AV nodes (though the SA node may be supplied by the LAD in approximately 40% of human hearts), the bundle of His (with assistance from the PDA and LAD), the entirety of the right atrium, and predominant parts of the right ventricle, posterior fascicle of the left bundle branch, and the interatrial septum. Regardless of dominance, the PDA (either as a branch of the RCA or LCA) generally supplies the superior-posterior interventricular septum, the left ventricular inferior wall, and the posterior papillary of the mitral valve. RCA occlusion causes ischemic changes in ECG leads II, III, and aVF.
Patrick J. Lynch, medical illustratorderivative work: Fred the Oyster (talk)adaption and further labeling: Mikael Häggström (Coronary.pdf) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons
Other References
- Wynn GJ, Noronha B, Burgess MI. Functional significance of the conus artery as a collateral to an occluded left anterior descending artery demonstrated by stress echocardiography. International Journal of Cardiology (2008). 140(1): e14–5. doi:10.1016/j.ijcard.2008.11.039 Link
- James TN. Anatomy of the Coronary Arteries in Health and Disease. Circulation. 1965; 32:1020-1033. doi:10.1161/01.CIR.32.6.1020 Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.