Copy link
Double-Lumen Endotracheal Tubes for One-Lung Ventilation
Last updated: 04/25/2023
Key Points
- The double-lumen endotracheal tube (DLT), a bifurcated tube with both an endotracheal and an endobronchial lumen, is a common technique to achieve lung separation in adults. The left-sided DLT is the most commonly used device for lung separation due to a greater margin of safety when compared to right-sided DLT.
- Key advantages of DLT over bronchial blockers include greater ease of use and once in position, less likelihood of dislodgment, and access to the isolated airway (e.g., for suctioning).
- Disadvantages of DLT include difficulty of placement during laryngoscopy and risk of tracheal or bronchial injury.
Indications for Lung Separation
- Lung separation techniques are designed to facilitate surgical exposure and provide one-lung ventilation (OLV) in patients undergoing thoracic, esophageal, cardiac, vascular, or selective spine surgery.1 The most common indications for lung separation and OLV are:
1. To provide a still operative field and surgical exposure or for lung isolation
2. To prevent contamination of the contralateral lung from hemorrhagic or purulent material
3. To provide application of differential lung ventilation, such as continuous positive airway pressure to the nondependent lung and positive end-expiratory pressure to the dependent lung. - Lung separation in adults can be achieved with a DLT, which is a bifurcated tube with both an endotracheal and an endobronchial lumen and can be used to selectively achieve separation of either the right or left lung. The DLT can be used to selectively achieve separation of either the right or left lung. Currently, there are two versions of the DLT, a left and right-sided DLT, which are designated to accommodate the unique anatomy of each mainstem bronchus. Left-sided DLTs are common for their ease of use and positioning; however, right-sided DLTs are especially helpful for specific indications.
- Indications for right-sided DLT include:
- Descending thoracic aortic aneurysm compressing left mainstem bronchus
- Left-sided pneumonectomy or sleeve resection
- Any tumor compressing or distorting the anatomy of the left mainstem bronchus
Size Selection of the Double-Lumen Endotracheal Tubes
The ideal size DLT is one in which the main body of the tube passes without resistance through the glottis and advances easily within the trachea and in which the endobronchial lumen component passes into the selected bronchus without difficulty or resistance.
- A DLT that is too small in size requires a larger endobronchial cuff volume (i.e., >3.0 mL) to achieve blockade of the bronchus, which might increase the incidence of malposition. Also, too small DLT may migrate deeply into the bronchus resulting in airway trauma.
- An undersized DLT might present a higher resistance to gas flow and increase auto positive end-expiratory pressure.
- A DLT that is too large requires less endobronchial cuff volume (i.e., <1.0 mL) to achieve blockade of the bronchus. Large DLT can potentially produce damage to the airway, including lacerations or perforations.
- Currently, there is no data to demonstrate objectively a good method to select the optimal size.
- Some studies have selected the left-sided DLT based on the height and sex of the patient: 35 and 37 Fr for females and 39 and 41 Fr for males.
- Others have used radiological studies measuring the tracheal width or measurement of the tracheal diameter with an ultrasound in addition to patient height and sex.
Methods of Insertion of Double-Lumen Endotracheal Tubes
- Two techniques are most commonly used by anesthesiologists when inserting and placing a DLT: blind technique and bronchoscopy guidance technique. A comparison of the two techniques is shown in Figure 1.
- In the blind technique, the DLT is passed via direct or video laryngoscopy, then it is turned to the left (for a left-sided DLT) or right (for a right-sided DLT) after the endobronchial cuff has passed beyond the vocal cords. The DLT is then advanced until it reaches the depth of insertion at the teeth, which is approximately 29 cm for both men and women if the patient’s height is at least 170 cm.
- The other technique involves the use of a flexible fiberoptic bronchoscope as a guide to the selected main bronchus. After the tip of the endobronchial lumen of the DLT has been passed through the vocal cords under direct or video laryngoscopy, fiberoptic bronchoscopy is used to guide the DLT to the appropriate bronchus.
- The use of video laryngoscopy improves visualization of the DLTs at first pass at the glottis; however, there is a significant incidence of tracheal cuff rupture with the use of video-laryngoscopes (in part attributed to the hyperangulation of some video-laryngoscope designs, difficulty manipulating the DLT around the blade, or the focus of the laryngoscopist on a video screen. The Airtraq has reported no tracheal cuff rupture.
Placement Technique for a Left-Sided Double-Lumen Endotracheal Tube
- Placement and positioning of a left-sided DLT can be accomplished with either of the following techniques:
- In the blind technique, the left-sided DLT is passed beyond the vocal cords (endobronchial cuff) and the tube is rotated 90° counterclockwise and advanced until the tip of the tube enters the left mainstem bronchus (Figure 1).
- In the bronchoscopy guidance technique, the endobronchial tip is passed beyond the vocal cords and guided with the aid of the fiberoptic bronchoscope into the entrance of the left mainstem bronchus.2
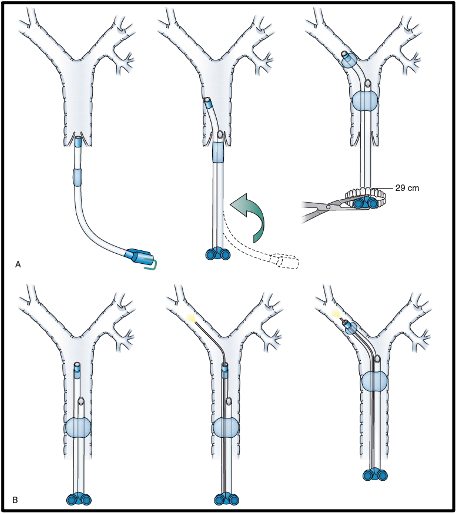
Figure 1. 1A shows the blind method technique and Figure 1B shows a flexible fiberoptic bronchoscopy guidance technique for placement of a left-sided DLT. A) A blind technique for placing a left-sided double-lumen tube (DLT). (Left) The DLT is passed with direct laryngoscopy passed the vocal cords. (Center) The DLT is rotated 90 degrees to the left. (Right) The DLT is advanced into the left mainstem bronchus, with a depth at the level of the teeth approximately to the 29 cm mark of the DLT. (B) A fiberoptic bronchoscopy–guidance technique for placing a left-sided DLT. (Left) The DLT is passed with direct laryngoscopy passed the vocal cords. (Center) The fiberoptic bronchoscope is advanced through the endobronchial lumen. The tracheal carina and the left main stem bronchus are visualized. (Right) The DLT is rotated 90 degrees to the left, and with the aid of the fiberoptic bronchoscope; the tube is advanced to the optimal position into the left main stem bronchus. Used with permission from Campos JH.1
- Fiberoptic bronchoscopy to confirm the optimal position of the left-sided DLT (see Figure 2). The optimal position for a left-sided DLT is confirmed with fiberoptic bronchoscopy through the tracheal lumen to observe a fully inflated endobronchial cuff with no more than 3 mL of air located at least 5 to 10 mm below the tracheal carina inside the left mainstem bronchus. The second important view is the endobronchial bronchoscopy view, where the fiberoptic bronchoscope is advanced inside the endobronchial lumen and the patency of the lumen is observed before advancing the bronchoscope through the blue portion of the tube. The next view is at the distal end of the endobronchial tip of the tube, where a clear and unobstructed view of the bronchial carina with a left upper and left lower lobe bronchus entrance orifices are visualized distally.
- To identify which is the right mainstem bronchus while placing a left-sided DLT, the fiberoptic bronchoscope is advanced through the tracheal lumen below the main tracheal carina to the right side approximately 1-2 cm, at which point the orifice of the right upper lobe (RUL) bronchus is seen at 3 to 4 o’clock on the lateral wall. By advancing the fiberoptic bronchoscope inside the right upper bronchus, it should display a clear view of three orifices (apical, anterior and posterior segments). This is the only structure of the tracheobronchial tree that has three orifices. Identifying the RUL orifice should be part of the routine bronchoscopy in thoracic anesthesia.
Figure 2 shows the optimal position of a left-side DLT as seen with a fiberoptic bronchoscope.
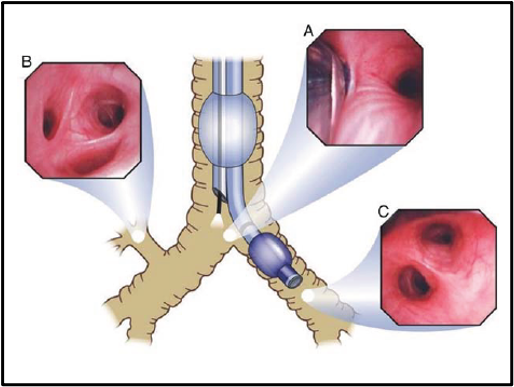
Figure 2. The optimal position of the left-sided double-lumen tube (DLT), as seen with a fiberoptic bronchoscope. (A) View from the tracheal lumen of the unobstructed entrance of the right mainstem bronchus. (B) View from the tracheal lumen of the right upper bronchus. (C) View from the bronchial lumen of the left upper (above) and left lower (below) lobe bronchi. Used with permission from Campos JH.3
Right-Sided Double-Lumen Endotracheal Tubes
- The preferred technique for placement of the right-sided DLT is with the fiberoptic bronchoscopy guidance technique. After the right-sided DLT is passed beyond the vocal cords under direct laryngoscopy, the fiberoptic bronchoscope is advanced through the endobronchial lumen. Before advancing the DLT, the tracheal carina and the entrance of the right mainstem bronchus are identified, then the DLT is rotated 90° to the right and advanced with the aid of the fiberoptic bronchoscope. The optimal position of a right-sided DLT is one that provides good alignment between the endobronchial lumen opening slot and visualized the three segments of the RUL bronchus. A clear view of the bronchus intermedius and the right lower lobe bronchus should be seen from the endobronchial lumen From the tracheal view, the optimal position for a right-sided DLT provides a view of the edge of the blue cuff of the endobronchial balloon when inflated just below tracheal carina and a full view of the entrance of the left mainstem bronchus. Figure 3 shows the optimal position of a right-sided DLT seen from the endobronchial or endotracheal view with a fiberoptic bronchoscope.
- The fiberoptic bronchoscopic examination should be performed with the patient in the supine position, after turning into the lateral decubitus position, or whenever it is needed during the case (i.e., malposition or inspection of stapling line).
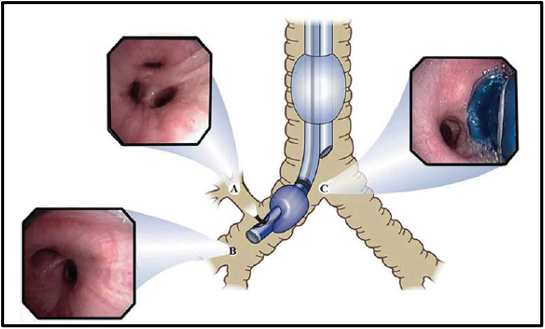
Figure 3. The optimal position of a right-sided double-lumen endotracheal tube. (A) Shows the take-off of the right-upper bronchus with three segments (apical, anterior, and posterior) when the fiberoptic bronchoscope emerges from the opening slot located in the endobronchial lumen. (B) Shows an unobstructed view of the entrance of the right middle and right lower lobe bronchus when the fiberscope is passed through the endobronchial lumen. (C) Shows a view of tracheal carina to the right edge of the blue balloon fully inflated, and to the left, an unobstructed view of the entrance of the left-mainstem bronchus when the fiberscope is advanced through the tracheal lumen. Used with permission from Campos JH.2
Advantages and Disadvantages of Double-Lumen Endotracheal Tubes
Advantages of the DLT
- A large internal lumen diameter facilitates suctioning compared to bronchial blockers.
- DLT is the best device for absolute indications for lung separation to protect the lung from soiling or establishment of continuity of the airway.
- Empyema, purulent secretions, or pulmonary hemorrhage
- Lung lavage
- Bronchopleural fistula
- Conversion from two-lung to one-lung ventilation and back is easy and reliable.
Disadvantages of the DLT
- Difficulties in selecting the proper size
- More difficult to place during laryngoscopy compared to single lumen endotracheal tube
- Potential damage to the tracheal cuff during intubation
- Major tracheobronchial injuries (rare)
Specialized Double-Lumen Endotracheal Tubes
- In addition to conventional DLTs, several modifications have been made to develop specialized DLTs to improve the quality of placement and patient safety.
- The VivaSight® DLT (Ambu, Inc., Maryland, USA) utilizes a camera and light source embedded into the DLT at the distal opening of the tracheal lumen to provide continuous visualization of the airway. Positioned between the tracheal and bronchial cuffs, the integrated camera provides live video of the airway to guide DLT placement and to monitor tube position during lung isolation.4 Figure 4 displays the VivaSight® DLT.
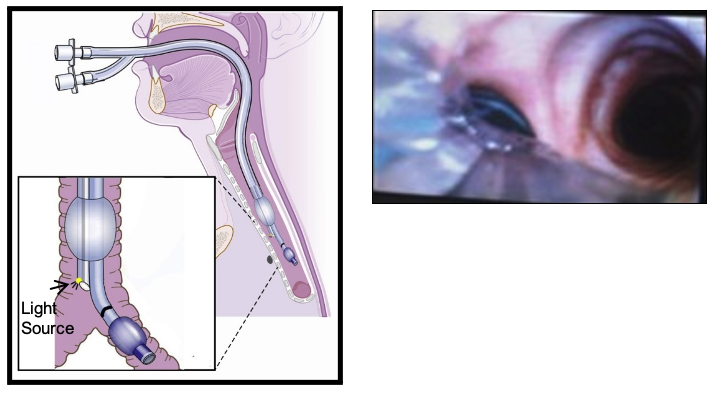
Figure 4. A left-sided VivaSight DLT® along with an image of the optimal position when connected to a monitor camera. DLT, Double-lumen tube. Used with permission from Campos JH.4
- Another DLT, the ECOM® Double Lumen Endobronchial Tube (ECOM Medical, Inc., California, USA), utilizes additional features to function as an endotracheal cardiac output monitor. An array of flexible surface electrodes attached to the endotracheal cuff and shaft of the DLT measures bioimpedance in the ascending aorta. A corresponding ECOM® monitor incorporates input from arterial blood pressure monitoring (e.g., via existing radial arterial catheter) to derive cardiac output, stroke volume, and systemic vascular resistance, which are displayed continuously. Figure 5 displays the ECOM® DLT.
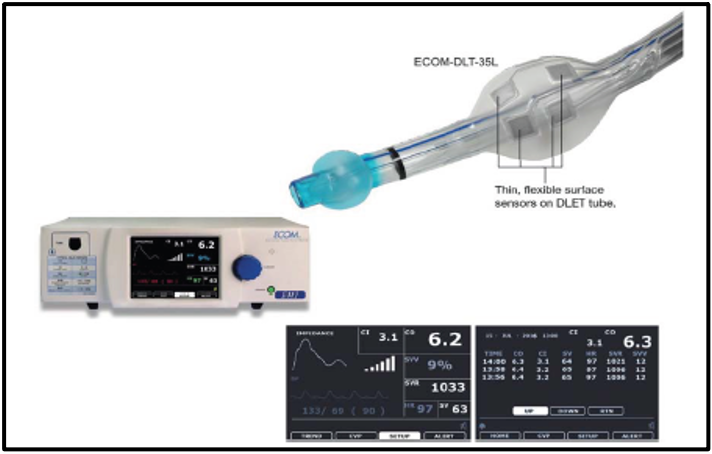
Figure 5. The ECOM-DLT has multiple electrodes on the cuff and the tube that continuously measure the bioimpedance signal from the ascending aorta with measurements of cardiac output. DLT, Double-lumen tube. Used with permission from Campos JH.1
References
- Campos JH. Separation of the lung: Double-lumen endotracheal tubes and endobronchial blocker. In: Cohen E (ed). Cohen's Comprehensive Thoracic Anesthesia. 1st edition. Philadelphia, PA. Elsevier. 2022: 213-39.
- Campos J. Fiberoptic bronchoscopy for positioning double-lumen tubes and bronchial blockers. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. 2nd edition. Switzerland. Springer Nature. 2019:311-22.
- Campos JH. Current techniques for perioperative lung isolation in adults. Anesthesiology 2002; 97:1295-1301. PubMed
- Campos J, Hanada S. DLT with incorporated fiberoptic bronchoscopy. In: Rosenblatt WH, Popescu WM (eds). Master Techniques in Upper and Lower Airway Management. Philadelphia, PA. Wolters Kluwer. 2015: 250-1.
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.