Copy link
Epidural and Combined Spinal-Epidural: Anatomy, Indications, and Physiological Effects
Last updated: 12/19/2023
Key Points
- Combined spinal-epidural (CSE) anesthetics can often be used as the sole anesthetic, whereas epidurals alone are usually insufficient (with a few exceptions, notably labor) and are often used as an adjunct to general anesthesia.
- Absolute contraindications to neuraxial anesthesia include patient refusal, allergy to medication used, infection at the site, and severe coagulation abnormalities.
- Physiologic effects of neuraxial anesthesia can be profound and are related to the blockade of autonomic fibers.
Anatomy
- The vertebral column consists of 33 bones, including 7 cervical, 12 thoracic, 5 lumbar, 5 fused sacral, and 3 to 5 (most commonly 4) fused coccygeal vertebrae.1-3
- Spinal anesthetics target the lumbar and caudal regions, whereas epidurals have a wider range of applicability and include the thoracic space.
- Ligaments provide support and stability for the spinal column. These structures are typically thicker and stronger lower in the column. Notably, the ligamentum flavum, a longitudinal structure along the dorsal spinal column, is thicker and more complete in the lumbar region.1,2
- The spinal cord thins from a cranial to caudal direction, with the cord terminating in adults at L1 or L2 and the dural sac at S2 (Figure 1). As a result, the epidural space grows from a cranial to caudal direction and is largest in size in the lumbar region.2
- The epidural space exists both anterior and posterior to the cord, comprised of fat, lymphatics, and venous plexuses. Adhesions and fibrous changes can develop in patients who have had epidurals previously, which can affect access and medication spread.2
- The depth of the epidural space is greatest in the lumbar spine, averaging approximately 6 cm from skin to ligamentum flavum (4-5 cm in thoracic spine) in adults.3
- The epidural space is bounded by the bony structures of the spinal column, excludes the contents of the dura, and communicates with the paravertebral spaces via the spinal foramina, from which the nerve roots exit.
- The Artery of Adamkiewicz (supplying the anterior spinal cord) is highly variable but most commonly enters the canal at the left L1 foramen.1-3
- The internal venous plexus, which drains the cord, is prominent in the lateral epidural space and ultimately empties into the azygous system.3
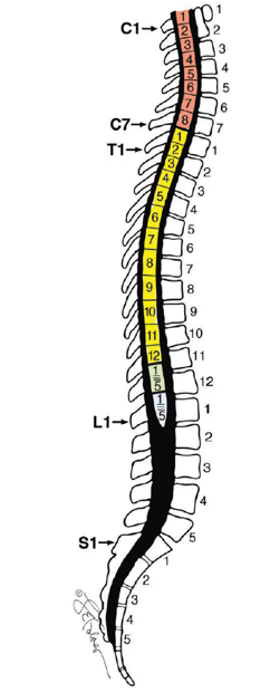
Figure 1: Relationship between the spinal cord and vertebral bodies. Used with permission from Loo NH, et al. AA Case Rep. 2017; 9(16):164-8.
Indications and Contraindications
Indications
- Epidurals can be used as the primary anesthetic, usually via a combined spinal-epidural (CSE), for procedures involving the lower half of the body.
- Epidurals can also be used as an adjunct to general anesthesia for intraoperative and postoperative analgesia for thoracic, abdominal, or lower extremity surgery.
- An exception is during obstetric anesthesia, where high-volume (often 20mL or more) epidurals can be used as the primary anesthetic.
- Evolving evidence suggests that epidurals may be of particular benefit for patients undergoing thoracic/upper abdominal surgery at risk for postoperative pulmonary complications and postoperative ileus.3
Contraindications3
- Absolute contraindications:
- Patient refusal, allergy to medication used, infection at the site, and severe coagulation abnormalities
- Critical/severe aortic stenosis and high intracranial pressure
- Spinal tumors near the level of approach
- Relative contraindications:
- Spinal abnormalities, previous spine surgery at the desired target, coagulopathy, fixed cardiac output states, and active infections
- Autoimmune neurologic disorders may pose an undue risk, and careful consideration of risks and benefits must be weighed.
Physiological Effects of Spinal Anesthesia
- In general, the physiological effects will depend on the site of neural blockade, and how far along the sympathetic chain the neural transmission is interrupted. Blockade of autonomic fibers (up to 6 levels above the site of injection) results in many of the side effects seen in other body systems.
Central Nervous System
- Sensory changes occur within seconds, followed by loss of proprioception and motor function. Patients typically describe perineal then lower limb sensory changes (typically warmth) within minutes of epidural anesthetic injection. This is followed by loss of temperature, pain, and two-point discrimination, then loss of vibration sense, proprioception, and motor function over several more minutes. Pressure, proprioception, and motor functions may be retained despite surgical anesthesia. These are signs of a less dense neural blockade. The rate of sensory changes is slower than that of spinal anesthesia; neurologic changes within seconds should signal a possible intrathecal catheter placement.
Cardiovascular
- Most patients do not experience large swings in heart rate after epidurals, though reflex tachycardia can follow decreased blood pressure. Cardioaccelerator fibers (T1-T4 sympathetic fibers) may be somewhat affected by thoracic epidurals, with a slight reduction in heart rate4, though this is more common with spinals. Significant bradycardia or cardiovascular collapse with a small epidural dose (e.g. 5 mL) may be a sign of intrathecal catheter placement.
- Hypotension is common. Rapid reduction in afterload and preload occurs due to the blockade of sympathetic autonomic fibers, with resultant vasodilation and venodilation.4
- Cardiovascular collapse within seconds may result in patients with limited functional reserve due to these hemodynamic changes.
- Local anesthetic toxicity results in prolonged cardiac arrest due to complex effects on myocardial lipid metabolism (though this is unlikely given typical doses in epidural and CSE techniques).
Pulmonary
- Neuraxial blockade impairs respiratory muscle function in a level-dependent fashion.
- Abdominal and intercostal muscle weakness from epidurals can result in the reduction in peak expiratory pressure. Forced expiratory volume in the first second, forced vital capacity, and vital capacity may also be reduced to a lesser degree.4
- Patients may experience subjective shortness of breath secondary to proprioceptive blockade of afferent fibers from the abdominal and chest walls.
- Block height reaching C3-5 directly impairs phrenic nerve function, resulting in diaphragm weakness requiring urgent airway management and ventilation, though this is rare with thoracic/lumbar epidurals.
- Neuraxial opioids may induce hypoventilation that may be prolonged.
Musculoskeletal
- Neuraxial anesthesia has a wide range of direct and indirect effects on the musculoskeletal system.3,4
- Impaired thermoregulation may result in involuntary shivering.
- Spinal anesthesia provides excellent muscle relaxation for lower abdominal and lower extremity surgery.
Gastrointestinal
- Neuraxial anesthesia leading to sympathectomy results in increased parasympathetic tone.4
- Nausea and vomiting may occur from hypotension (especially in obstetrics) or from increased gut motility, increased secretions, and reduced sphincter tone.
- Increased gut motility may reduce the risk of postoperative ileus common with abdominal surgeries.
Renal
- Blockade of S3 can cause inhibition of bladder detrusor function, leading to urinary retention.3
- Prolonged blockade of detrusor function may lead to bladder distension or rupture in very rare cases.
- Acute kidney injury can result from prolonged hypotension and diminished renal perfusion.
Hematology
- There is evidence for reduced blood loss in orthopedic, gynecologic, obstetric, and urologic procedures due to reduced mean arterial pressure, peripheral vasodilation, and redistribution of blood away from the operative site.4
- Reduction in rates of deep vein thrombosis and pulmonary embolism is possible following total hip and total knee replacements, likely secondary to increased blood flow to lower extremities and prevention of the hypercoagulable state seen with general anesthesia.
References
- Bican O, Minagar A, Pruitt AA. The spinal cord: a review of functional neuroanatomy. Neurol Clin. 2013;31(1):1-18. PubMed
- Macpherson D, Quondamatteo F, Broom M. Update on applied epidural anatomy. BJA Educ. 2022;22(5):182-189. PubMed
- Gerheuser F, Roth A. Periduralanästhesie [Epidural anesthesia]. Anaesthesist. 2007 ;56(5):499-523; quiz 524-6. German. PubMed
- Grass JA. The role of epidural anesthesia and analgesia in postoperative outcome. Anesthesiol Clin North Am. 2000;18(2):407-28. PubMed
- Papper EM. Spinal and epidural anesthesia. Effects on renal function. Acta Anaesthesiol Scand Suppl.1966; 24:105-10. PubMed
Other References
- Toledano R, Van de Velde M. Epidural Anesthesia and Analgesia. New York School of Regional Anesthesia. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.