Copy link
Hepatopulmonary Syndrome
Last updated: 05/09/2023
Key Points
- Hepatopulmonary syndrome (HPS) is characterized by intrapulmonary vascular dilatations in the setting of portal hypertension, leading to right-to-left shunts and hypoxia.
- It is the most common pulmonary vascular disorder associated with liver disease, with portopulmonary hypertension (PPH) occurring less frequently.
- Patients with HPS typically present with hypoxia.
- The only currently approved treatment for HPS is supplemental oxygen.
- Patients with HPS have good outcomes after liver transplantation (LT), with similar 5-year survival rates compared to all patients after LT.
Introduction
- HPS is present in about 5-32% of LT candidates with cirrhosis or end-stage liver disease.1
- Reports of incidence vary widely due to historically variable diagnostic criteria. In 2001, the European Respiratory Society developed the Pulmonary-Hepatic Vascular Disorders task force to develop consensus criteria for the diagnosis and management of HPS and PPH.2
- The severity of liver disease or portal hypertension does not predict the presence or severity of HPS.
- The most common presenting symptom in patients with HPS is worsening dyspnea and hypoxia. Orthodeoxia (oxygen desaturation with movement from supine to upright position) and platypnea (dyspnea with movement from supine to upright position) may also be present.
- The mainstay of treatment for HPS is supplemental oxygen. HPS can often be reversed completely with successful LT.
Pathogenesis
- Patients with portal hypertension have a hyperdynamic circulation, with high cardiac output resulting in splanchnic volume overload and bowel wall edema, which leads to bacterial translocation and the subsequent release of cytokines and endotoxins into the systemic circulation.
- Endotoxemia and bacterial translocation leads to the activation of macrophages and monocytes in the lungs, causing the accumulation and/or activation of cytotoxic and vasodilatory mediators such as nitric oxide, tumor necrosis factor-alpha, carbon monoxide, and endothelin which contribute to the development of abnormal pulmonary vascular dilatation.
- Pulmonary vascular dilatation occurs due to increased shear stress on a normally low resistance system, a compensatory mechanism to maintain normal pulmonary vascular resistance. This is the hallmark of HPS, which must be differentiated from PPH (a vasoconstrictive phenomenon) in patients with cirrhosis and pulmonary symptoms (Figure 1).
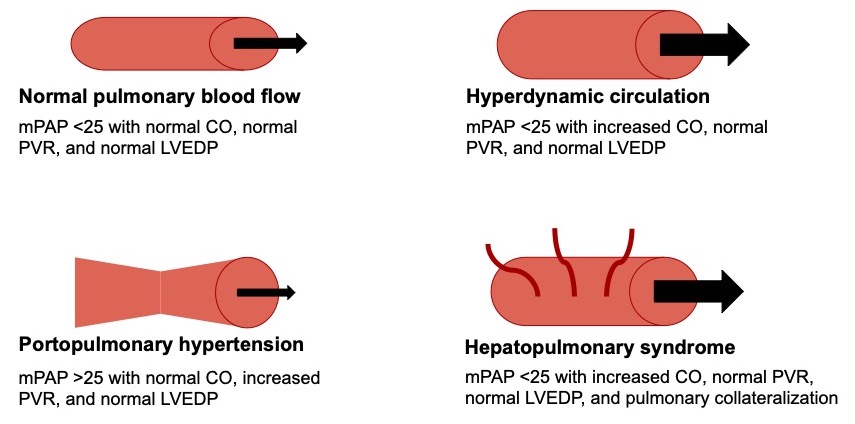
Figure 1. Differentiating HPS from PPH and high-flow states. Normal parameters: CO 4-8 L/min. PVR < 3 Wood units. LVEDP ≤ 15 mmHg. Abbreviations: mPAP = mean pulmonary artery pressure, CO = cardiac output, PVR = pulmonary vascular resistance, LVEDP = left ventricular end diastolic pressure.
- Marked pulmonary dilatation may also be accompanied by collateralization and abnormal arteriovenous connections.
- HPS is a state of ventilation-perfusion mismatch. Increased perfusion secondary to vascular dilatation and collateralization in the setting of preserved ventilation results in the right-to-left shunting of blood (Figure 2).
- Hypoxia in HPS is worsened by partial impairment of the normal compensatory mechanism – hypoxic pulmonary vasoconstriction (HPV). The abnormally dilated pulmonary vasculature has reduced tone and does not respond normally to hypoxic states, worsening the right-to-left shunt.
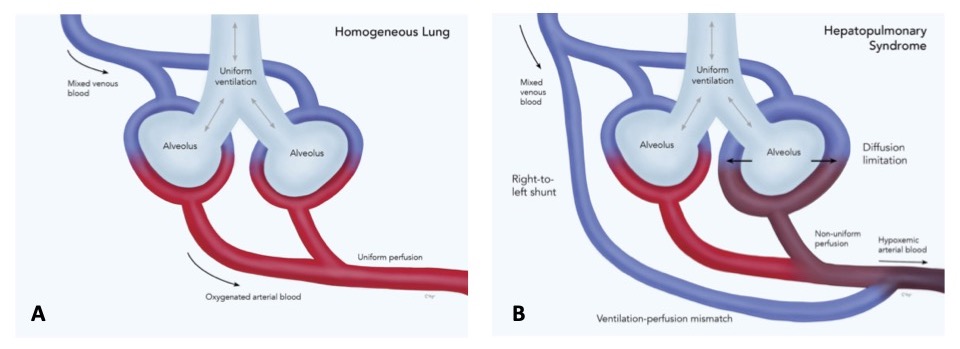
Figure 2. Pathophysiology of hypoxemia in HPS. Ventilation and perfusion are balanced in the homogenous (healthy) lung (panel 1), whereas ventilation-perfusion mismatch occurs in HPS (panel B). Adapted from Rodríguez-Roisin R, et al. N Engl J Med. 2008;358(22):2378-87.1
Diagnosis & Management3
- Diagnosis requires the presence of the following:
- portal hypertension with or without cirrhosis or end-stage liver disease;
- oxygenation defect;
- PaO2 < 80 mmHg; OR
- alveolar-arterial oxygen gradient ≥ 15 mmHg while breathing room air;
- pulmonary vascular dilatation.
- Workup typically includes:
- Pulse oximetry
- Arterial blood gas
- Contrast echocardiography
- It is used to identify the late arrival of bubbles (4-6 cardiac cycles), suggesting an intrapulmonary shunt.
- The early arrival of bubbles (1-3 cardiac cycles) suggests an intracardiac shunt and should raise suspicion for a patent foramen ovale or an atrial septal defect as a potential etiology of hypoxia.
- Radionuclide scanning with 99mTc albumin
- Macroaggregated albumin is typically too large to pass through the pulmonary circulation, and its uptake in the brain can be quantitatively measured, with an increased presence in the brain correlating with greater degrees of pulmonary dilatation.
- Pulmonary angiography is rarely performed. It is only utilized if there is a high suspicion for arteriovenous communications that may be amenable to embolization.
- Medical management is currently limited to supplemental oxygen. Early research on targeted therapies is ongoing, based theoretically on the pathophysiology of increased NO synthesis, TNF-alpha involvement, and activation of endothelin-B receptors.4
- Liver transplantation is the only known cure for HPS.
Prognosis
- In LT patients with all degrees of HPS, 5-year survival has been reported to be 76%, compared to 23% for patients with HPS who did not undergo LT.5
- The reported perioperative mortality for patients with HPS after LT is between 8 and 16%.6
- Patients with a pretransplant PaO2 ≤ 50 mmHg have significantly increased mortality associated with LT.
- Patients with HPS typically have a progressive decline in PaO2 over time. This has led to additional Model for End-stage Liver Disease points (MELD: a scoring system utilized for organ allocation) given for HPS to expedite access to transplantation prior to reaching this PaO2 cutoff.
References
- Rodríguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome--a liver-induced lung vascular disorder. N Engl J Med. 2008;358(22):2378-87. PubMed
- Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB; ERS Task Force Pulmonary-Hepatic Vascular Disorders (PHD) Scientific Committee. Pulmonary-Hepatic vascular Disorders (PHD). Eur Respir J. 2004;24(5):861-80. PubMed
- Hoeper MM, Krowka MJ, Strassburg CP. Portopulmonary hypertension and hepatopulmonary syndrome. Lancet. 2004;363(9419):1461-8. PubMed
- Eshraghian A, Kamyab AA, Yoon SK. Pharmacological treatment for hepatopulmonary syndrome. Biomed Res Int. 2013:670139. PubMed
- Swanson KL, Wiesner RH, Krowka MJ. Natural history of hepatopulmonary syndrome: Impact of liver transplantation. Hepatology. 2005;41(5):1122-9. PubMed
- Krowka MJ, Mandell MS, Ramsay MA, et al. Hepatopulmonary syndrome and portopulmonary hypertension: a report of the multicenter liver transplant database. Liver Transpl. 2004 Feb;10(2):174-82. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.