Copy link
Mediastinal Masses: Adults, Mediastinoscopy
Last updated: 11/10/2023
Key Points
- Anterior mediastinal masses can compromise the airway and cardiovascular system by a compression mechanism.
- The anatomic location and size have significant implications for the trachea, bronchus, and major vessels.
- Anesthesia considerations are based on specific mass size and surgical technique, i.e., for a thoracotomy, lung isolation devices are recommended.
Pathophysiology
- Although anterior and posterior mediastinal masses are uncommon in adults, they present significant challenges to the anesthesiologist because of their impact on the airway and cardiovascular system.
- The anatomic location and size of the mediastinal mass have significant implications related to compression of the airway, mainly in the lower third of the trachea and main bronchi, and compression of the major vessels, including superior vena cava, pulmonary vessels, and adjacent organs.1
- Airway compression can occur when the patient is placed supine, at induction of anesthesia, intraoperatively, at extubation, or in the postoperative period.
- Compression of the large airways can manifest with significant changes in gas exchange and patient morbidity. Patients with large anterior mediastinal masses develop severe hypoxemia caused by a total obstruction of the left main bronchus and pulmonary artery compression.
- Another potential complication related to airway obstruction is the development of noncardiogenic pulmonary edema, particularly in patients with severe airway obstruction either before or after surgical interventions.
- Pulmonary function tests (PFTs) should be obtained in the patient with an anterior mediastinal mass to clarify the impact on the airway. The PFTs provide a dynamic assessment of airway obstruction throughout the respiratory cycle. The flow volume loop (FVL) is probably the most helpful in identifying the presence of an upper airway obstruction. Interpretation of the FVL is critical to define the extent of airway obstruction caused by the mass and to determine if the obstruction is inspiratory, expiratory, or both. A plateau in the inspiratory flow of the FVL is consistent with a variable extrathoracic upper airway obstruction. A plateau in the expiratory flow with a normal inspiratory flow suggests an intrathoracic upper airway obstruction. In contrast, patients who have flattening of both the inspiratory and expiratory flows have a pattern indicative of a fixed obstruction. Figure 1 shows the different patterns of FVL.
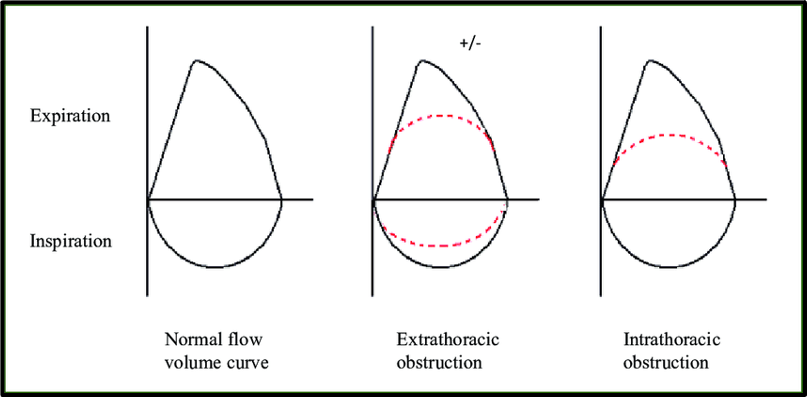
Figure 1. Flow volume loops. A) normal, B) extrathoracic obstruction C) intrathoracic obstruction
- Anesthesiologists have requested upright and supine spirometry as a part of the preoperative assessment in patients with an anterior mediastinal mass. A retrospective cohort study of adults with known mediastinal masses identified 37 patients who had spirometry ordered as a part of their preoperative assessment.2 The overall mean values reported in a seated position include forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) of 4.02 ± 0.75 L (90.7 ± 13.3% predicted volume) and 3.22 ± 0.56 L (89.6 ± 14.2% predicted volume), respectively. Only ten patients had both upright and supine spirometry ordered, including four who had abnormal results suggestive of upper airway obstruction. Of the patients who had upright and supine spirometry performed, the test was ordered more commonly in the younger and symptomatic patients. Perioperative complications did not significantly occur more frequently in the patients who had upright and supine spirometry ordered than in those who did not have these tests performed. Although the results of spirometry were abnormal in four patients, suggesting upper airway obstruction, all received general anesthesia; no airway collapse, obstruction, or other perioperative complications occurred while receiving general anesthesia. The perioperative complications rate was 5.4%. The study did not demonstrate any correlation between abnormal upright and supine spirometry results and symptoms, with abnormal chest CT scan findings, or with the anesthetic technique, or the development of intra- and/or postoperative complications. Therefore, upright and supine spirometry may not be any better in predicting complications than are symptoms and chest CT scan and should not be routinely obtained in patients with anterior mediastinal masses.
- The initial study in patients with a suspected anterior mediastinal mass generally is a standard biplane chest radiography, which will identify up to 97% of mediastinal tumors. The chest x-ray also provides important information regarding the size and location of the mass.3 In addition, in this patient group in particular, special attention must be paid to the lateral radiograph of the chest to determine the overall extent of the mass and potential involvement of adjacent structures. A barium contrast esophagogram will also be useful to determine whether there is tracheobronchial tree involvement, although other dynamic studies may be more useful in defining the characteristics of the mass. An anterior mediastinal mass can be seen clearly in the left hemithorax of the posterior–anterior chest radiograph of Figure 2A. A lateral radiograph with esophageal contrast shows a mediastinal mass without compromise to the tracheobronchial tree in Figure 2B.
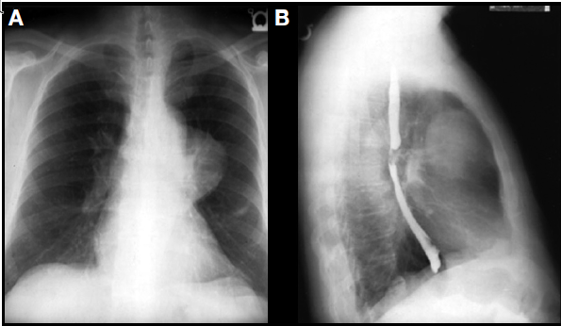
Figure 2. A: Anterior mediastinal mass in the left hemithorax of a posterior– anterior chest radiograph. B: Mediastinal mass without compromise to the tracheobronchial tree shown in a lateral radiograph with esophageal contrast.
- Another study useful in patients with mediastinal mass is the computed tomography (CT) scan of the chest that allows an appreciation of the size of the mediastinal mass and involvement of adjacent structures. Figure 3 shows a CT scan of the chest showing a large mediastinal mass on the left hemithorax.
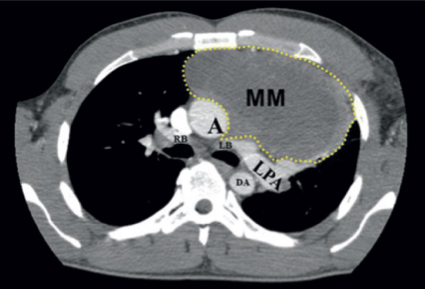
Figure 3. Anatomic location of the mediastinal mass in relation to airway and great vessels. Abbreviations: MM = mediastinal mass; A = aorta; LPA = left pulmonary artery; DA = descending aorta; LB = left bronchus; RB = right bronchus
Vascular Assessment of Mediastinal Mass
- Large tumors, especially in the mediastinum, can be highly vascularized, complicating surgical resection.
- Blood supply to mediastinal masses has been reported to be highly variable, possibly derived from branches from the internal mammary artery, bronchial arteries, intercostal vessels, pulmonary artery, and even coronary arteries. These large feeding vessels may cause technical and bleeding complications during surgical resection.
- A magnetic resonance imaging or high-resolution CT scan with intravenous contrast with multiplanar reconstruction is desirable.
- Tumors involving the mediastinum, especially large masses, have the potential to invade the great vessels such as the superior vena cava.
- In the setting of compression or invasion of the vena cava by large mediastinal tumors, the venous circulation will be maintained through collateral vessels. Contrast-enhanced, high-resolution CT with multiplanar and 3D reconstruction is an excellent technique in portraying the collateral circulation to facilitate an optimal surgery.4
Mediastinoscopy
- Mediastinoscopy is the traditional method for the evaluation of mediastinal lymph nodes in the staging of nonsmall cell lung cancer. It has largely been replaced for most patients by a combination of positron-emission tomography scans and endobronchial ultrasound-guided biopsies. In addition, mediastinoscopy is used to aid in the diagnosis of anterior/superior mediastinal masses.5
- The most common mediastinal diagnostic procedure is a cervical mediastinoscopy, in which a small transverse incision (2-3 cm) is made in the midline of the lower neck in the suprasternal notch. The pretracheal fascial plane is dissected bluntly and the mediastinoscope is inserted towards the carina. An alternative procedure is a parasternal (or anterior) mediastinoscopy with a small incision made through the interchondral space or the space of the excised second costal cartilage. Morbidity related to mediastinoscopy ranges from 2% to 8%.
- The most severe complication of mediastinoscopy is major hemorrhage,6 which may require emergent thoracotomy. Other potential complications include airway obstruction, compression of the innominate artery, pneumothorax, paresis of the recurrent laryngeal, phrenic nerve injury, esophageal injury, chylothorax, and air embolism.
Anesthesia Considerations
- Two large bore intravenous lines and an arterial line catheter should be used while managing a patient with a large mediastinal mass. In addition, if there is an involvement of the superior vena cava, a large intravenous catheter can be placed in the femoral vein or a large vessel in the lower extremity. In selective cases, a central venous pressure line monitor should be used because of the potential for a major hemorrhage to occur.
- Airway management will be determined based on an understanding of the presence and degree of airway compression and the surgical approach. Patients with a large anterior mediastinal mass who require general anesthesia have the potential for airway collapse. If the preoperative evaluation demonstrates major airway compromise, an awake intubation should be attempted with minimal sedation while maintaining spontaneous ventilation. A rigid bronchoscope and an experienced bronchoscopist must be available in the operating room prior to airway manipulation. The advantage of a rigid bronchoscope is that it can bypass the obstruction and provide a ventilation pathway if complete airway compression occurs.
- The type of endotracheal tube (ETT) used to manage the airway depends on the surgical approach. If a sternotomy is planned, a single-lumen ETT will be used. If a patient requires thoracotomy, once the airway is secure with a single-lumen ETT, a bronchial blocker can be used to facilitate lung isolation. In some cases, an armored single-lumen ETT is useful to prevent tube compression with subsequent inability to ventilate.
- Patients with an anterior mediastinal mass undergoing open thoracotomy will require lung isolation to facilitate surgical exposure. If the patient requires an awake intubation, a single-lumen ETT should be placed using a flexible fiberoptic bronchoscope. Once the airway is secure, a bronchial blocker can be used to occlude the desired bronchus. The advantage of using a blocker is that if postoperative mechanical ventilation is needed, its removal will allow the ETT to be kept in place.
- For the patient with a distal extrathoracic lesion that is causing compression of a bronchus, a left- or right-sided double-lumen endotracheal tube (DLT) may be more appropriate. In this situation, the DLT has several advantages, including the increased tube length, which allows bypassing the point of obstruction, and the ability to independently ventilate each lung. Special attention should be given to patients who have a tracheal or bronchial stent due to the potential to dislodge it while placing the ETT.
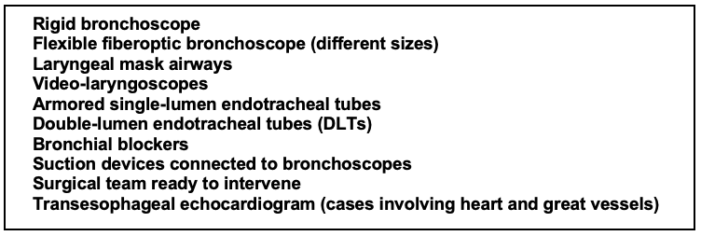
Table 1. The basic components for managing the airway in patients with a large anterior mediastinal mass
- Patients with thymomas may develop myasthenia gravis (MG). These patients with MG require special management because it is an autoimmune disorder of the neuromuscular junction. The muscle-type nicotinic receptors are destroyed by autoantibodies, resulting in muscle weakness and fatigue.
- Patients taking anticholinesterase or steroid therapy should continue them until the day of surgery. If the patient has a mediastinal mass that is not compressing the airway, then succinylcholine can be used for intubation. Nondepolarizing neuromuscular blockers should be used with caution in patients with MG due to their unpredictable effects. A quantitative neuromuscular blockade monitor must be used in order to administer the appropriate dose of muscle relaxants and evaluate complete reversal. Successful tracheal extubation can be accomplished in patients with MG who have received rocuronium after reversal with sugammadex.7,8 Extubation should be performed only when the patient is completely reversed from neuromuscular blockade.
- Tracheal extubation after the removal of a large mediastinal mass can present significant challenges. Some patients will experience tracheomalacia and might need to remain intubated in the early postoperative period. One study demonstrated that if the preoperative CT scan shows more than 50% tracheal compression and a mixed obstructive and restrictive pattern on PFTs, the likelihood for postoperative reintubation is high. Therefore, all intubating equipment should be available at the bedside, including a videolaryngoscope, supraglottic airways, and a flexible fiberoptic bronchoscope.
References
- Campos J. Airway management for a large anterior mediastinal mass resection. In: Rosenblatt WH, Popescu WM, eds. Master techniques in upper and lower airway management. LWW; 2015:296-299.
- Hnatiuk OW, Corcoran PC, Sierra A: Spirometry in surgery for anterior mediastinal masses. Chest 2001; 120:1152–6. PubMed
- Campos JH. Managing the patient with an anterior mediastinal mass in medically challenging patients undergoing cardiothoracic surgery. Cohen NH, ed. Society of Cardiovascular Anesthesiologists Monograph. 2009: 285-302.
- Li WW, van Boven WJ, Annema JT, et al. Management of large mediastinal masses: surgical and anesthesiological considerations. J Thorac Dis. 2016 Mar;8(3):E175-84. PubMed
- Slinger, PD, Campos JH. Anesthesia for Thoracic Surgery, Chapter. 53. In Miller’s Anesthesia, 9th ed. 2020: 1648-1716.
- Lohser J, Donington JS, Mitchell JD et al. Case 5--2005: Anesthetic management of major hemorrhage during mediastinoscopy. J Cardiothorac Vasc Anesth. 2005; 19:678-83. PubMed
- Campos JH, Peacher D. A new Post-thymectomy care algorithm—Post-anesthesia care unit vs. intensive care unit after robotic-assisted thoracoscopic surgery: Does it make a difference? J Cardiothorac Vasc Anesth. 2022; 36:3814-6. PubMed
- Sungur Ulke Z, Yavru A, Camci E, et al. Rocuronium and sugammadex in patients with myasthenia gravis undergoing thymectomy. Acta Anaesthesiol Scand 2013; 57:745–8. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.