Copy link
Myofascial Pain Syndrome and Trigger Point Injections
Last updated: 04/04/2023
Key Points
- Myofascial pain syndrome is a pain disorder characterized by chronic pain originating from myofascial trigger points and fascial constrictions.
- Trigger points are hyperirritable spots in the skeletal muscle that are identified via palpation and patient feedback, thus, is based on subjective information.
- Trigger point injections involve injecting a solution, often containing a local anesthetic with or without adjuvants, into the trigger point itself.
- The mechanism of action of trigger points remains unknown and systematic reviews have shown neither benefit or ineffectiveness.
- Trigger point injections should be part of an interdisciplinary approach, as recommended for all chronic nonmalignant pain syndromes.
Definition
- Myofascial pain syndrome is a pain disorder characterized by chronic pain originating from myofascial trigger points and fascial constrictions.1 The pain is typically associated with trigger points in muscles that radiate pain to the affected area when pressure is applied to them, even sometimes spontaneously without pressure. Pain can also be referred to what seems to be an unrelated part of the body.1
- The pain is typically described as a deep aching sensation, often with stiffness in the involved area. The pain is aggravated by the use of the involved muscle(s), psychological stressors, anxiety, cold, etc.1
- The pain is usually confined to a specific area with trigger points, which are differentiating factors from fibromyalgia. A single trigger point may progress to multiple points by persisting and causing neuroplastic changes at the level of the dorsal horn, which results in the amplification of the pain sensation (i.e., central sensitization) and expansion of pain beyond its original boundaries.1
Trigger Points
- Trigger points are hyperirritable spots in the skeletal muscle. There are no well-validated diagnostic criteria for the identification of trigger points. Defining characteristics of a trigger point are1
1. Focal point of tenderness to palpation of the muscle involved
2. Reproduction of pain complaint by trigger-point palpation (about 3 kg pressure)
3. Palpation reveals an induration of the adjacent muscle (the “taut band”).
4. Restricted range of movement in the muscle involved
5. Often pseudo-weakness of the muscle involved (no atrophy)
6. Often referred pain on continued (∼5 sec) pressure over the trigger point (Figure 1).
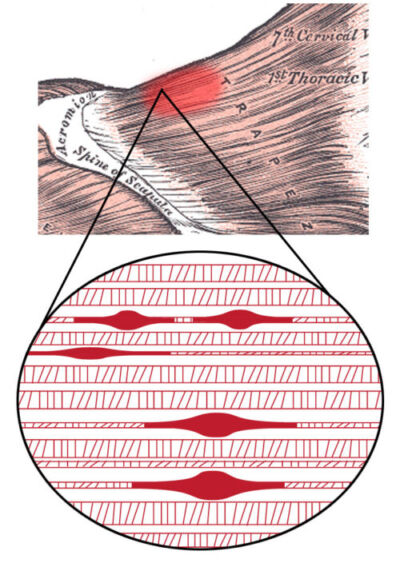
Figure 1. Myofascial trigger point in the trapezius muscle showing contraction knots within the taut band. Source: Wikipedia. Davidparmenter, CC BY-SA 3.0 Link.
- The diagnosis of an active trigger point requires appropriate palpation skills (Figure 2) and patient feedback; thus, much of the diagnosis is based on subjective information. Studies have shown that diagnostic reliability is dependent on skill and experience.
A thorough history is essential for diagnosis as the following predisposing factors are often present and contribute to trigger point formation:
- deconditioning
- poor posture
- repetitive mechanical stress
- psychological stressors
- mechanical imbalance (e.g., leg length inequality)
- joint disorders
- nonrestorative sleep
- vitamin deficiencies
Differential Diagnosis2
- Hypothyroidism
- Systemic lupus erythematosus
- Infections such as:
- Lyme disease
- Babesiosis
- Ehrlichiosis
- Candida albicans infections
- Parasitic diseases such as fascioliasis, amoebiasis, and giardia
- Myoadenylate deaminase deficiency
- Herpes zoster
- Hypoglycemia
- Systemic side effects of medications, including any of the statin drugs or even glucosamine sulfate
- Metabolic or nutritional deficiencies or insufficiencies of vitamin B12, vitamin D, and ferritin
Treatment
Myofascial pain syndrome is a chronic pain disorder that ideally should be managed with an interdisciplinary approach that involves physical, pharmacological, and psychological treatments.
- Correction of predisposing factors (listed above)
- Strengthening
- Medications
- No evidence of curative benefit from any medications
- Nonsteroidal anti-inflammatory drugs can provide some analgesia
- Tricyclic antidepressants can help with sleep disturbance and central sensitization
- Psychological treatments, as patients may develop anxiety and depression
- Trigger point injections
Trigger Point Injections
- Trigger point injections involve injecting a solution usually containing local anesthetics with or without steroids directly into a trigger point.
- They are also known as “wet needling,” versus dry needling, that involves only the insertion of a needle into the trigger point. Since the insertion of a needle can cause pain, addition of a local anesthetic solution can decrease this discomfort.
- The mechanism of action of trigger point injections in treating trigger points found in myofascial pain syndrome is still unknown.3
- A systematic review assessing the effectiveness of trigger point injections for chronic nonmalignant chronic pain found no clear evidence in the medical literature of either benefit or ineffectiveness.3
Technique for Trigger Point Injections4
- The patient should be placed in a recumbent position for the prevention of syncope and to assist with the relaxation of muscle tension.
- The trigger point should be identified by palpation.
- Utilizing a sterile technique, the skin overlying the trigger point should be grasped and the needle inserted 1-1.5 cm away from the trigger point so that the needle is advanced into the trigger point at a 30-degree angle with the goal of eliciting a local muscle twitch.
- The solution of choice should be injected.
- The process should be repeated by withdrawing the needle to the skin level and reinserting it into the trigger point until all sensitive foci are contacted.
- Following the procedure, the muscle group that was injected should undergo full active stretch.
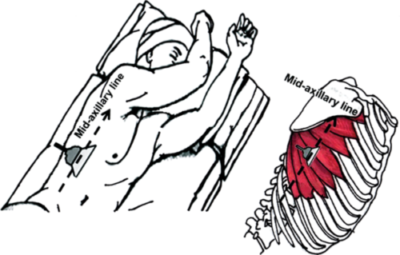
Figure 3. Anatomical considerations for trigger point injections in a patient with serratus anterior muscle pain syndrome, a specific type of myofascial pain syndrome. Used with permission from Vargas-Schaffer G, et al. A&A Practice. 2015;5(6):99-102.5
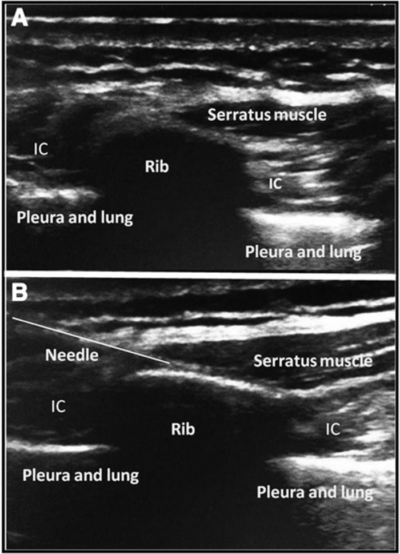
Figure 4. Ultrasound-guided infiltration of the serratus anterior muscle trigger point to treat serratus anterior muscle pain syndrome. Used with permission from Vargas-Schaffer G, et al. A&A Practice. 2015;5(6):99-102.5
References
- Bennett R. Myofascial pain syndromes and their evaluation. Best Pract Res Clin Rheumatol. 2007;21(3):427-45. PubMed
- Dommerholt J, Shah JP. Myofascial pain syndrome. In: Fishman, S. & Ballantyne, J. & Rathmell, J. Bonica’s Management of Pain (5th). Philadelphia, PA; Lippincott Williams & Wilkins; 2019: 504-525.
- Scott NA, Guo B, Barton PM, et al. Trigger point injections for chronic non-malignant musculoskeletal pain: a systematic review. Pain Med. 2009;10(1):54-69. PubMed
- Lavelle ED, Lavelle W, Smith HS. Myofascial trigger points. Anesthesiol Clin. 2007;25(4):841-51. PubMed
- Vargas-Schaffer G, Nowakowsky M, Eghtesadi M, et al. Ultrasound-guided trigger point injection for serratus anterior muscle pain syndrome: description of technique and case series. A&A Practice. 2015;5(6):99-102. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
