Copy link
Neonatal Assessment and Resuscitation
Last updated: 12/21/2023
Key Points
- Neonatal assessment is performed within 24 hours of birth to determine an infant’s well-being and the need for intervention.
- The Neonatal Resuscitation Program (NRP) was developed with a focus on effective ventilation to adequately resuscitate a newborn.
- Ventilation of the newborn’s lungs is the single most important and effective step in neonatal resuscitation, and an increase in heart rate is the most important indicator that effective ventilation is occurring.
- Positive pressure ventilation (PPV) at a rate of 40-60 inflations per minute is the primary method for providing support for newborns who are apneic, bradycardic, or demonstrate inadequate respiratory effort.
Introduction
- All newborns require an exam within the first 24 hours of birth to assess their general well-being and any concerns that may require intervention.
- The neonatal assessment begins with a head-to-toe exam, starting with the assessment of the newborn’s breathing and circulation, culminating in the determination of an APGAR score.1
- This initial screening includes positioning of the airway to ensure adequate ventilation, suctioning to clear secretions if needed, warming to maintain normothermia, and delayed cord clamping to reduce anemia.
- In neonates in whom there is concern for distress due to prematurity, difficult delivery, or physical exam of the newborn, fetal cord blood gases can be checked for further assessment.
- Finally, the NRP was developed by the American Academy of Pediatrics (AAP) as an evidence-based approach to resuscitate a neonate that is found to be in distress on initial assessment.2
APGAR Scoring
- The APGAR score was developed in 1952 by Dr. Virginia Apgar, an anesthesiologist at Columbia University.3
- It was initially developed as a quick method to assess the status of a neonate and assign a corresponding number that could be easily understood by others to represent the state of the newborn at 1 minute of life and the requirement for resuscitation.3
- Since its initial development, the APGAR score now incorporates an assessment at 1 minute and 5 minutes of life to assess the clinical status of the newborn and the response to resuscitative measures.3
- Since the development of the NRP, current recommendations state that the APGAR score should no longer be used to determine the need to begin resuscitation since resuscitation will often begin prior to 1 minute of life.2
- It is recommended that APGAR scoring be continued every 5 minutes for up to 20 minutes of life until an infant receives a score of at least 7.
- The scoring includes five components for assessment, with each component receiving a score of 0, 1, or 2 for a possible total of 103 (Table 1).
- A score of 7-10 is reassuring, with scores less than 7 requiring continued intervention and assessment.
- Of note, heart rate is considered the most critical part of the score in determining the need for further resuscitation efforts.3
- Please see the OA summary on APGAR score for more details. Link
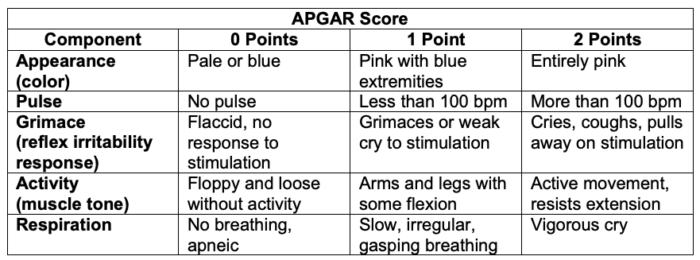
Table 1. The components of the APGAR score
Abbreviation: bpm = beats per minute
Neonatal Resuscitation Program
Overview
- The NRP algorithm was developed in 1987 and continues to be updated to provide an evidence-based approach to the resuscitation of neonates at birth.
- Approximately 10% of newborn infants need help beginning to breathe at birth, and about 1% need intensive resuscitative measures for cardiorespiratory function.2
- Neonatal mortality in the United States and Canada has decreased from 20 per 1000 live births in the 1960s to about 4 per 1000 live births today, with the majority of deaths and adverse outcomes caused by the inability of the neonate to establish or maintain adequate respiration.2
Key Points2
- The initial assessment includes an assessment of gestation, breathing, and tone.
- The initial interventions include drying and warming the baby, and providing tactile stimulation if the newborn is not breathing.
- Routine oral, nasal, oropharyngeal, or endotracheal suctioning is not recommended. Suctioning should be performed if PPV is required and the airway is obstructed.
- For nonvigorous newborns with meconium-stained amniotic fluid, routine laryngoscopy, with or without tracheal suctioning, is not recommended. Intubation and tracheal suctioning may be beneficial if there is airway obstruction during PPV.
- Effective ventilation is the mainstay of neonatal resuscitation. Continuous positive airway pressure, PPV, and oxygen support can be added to ensure adequate ventilation.
- PPV at a rate of 40-60 inflations per minute is the primary method for providing support for newborns who are apneic, bradycardic, or demonstrate inadequate respiratory effort.
- PPV should be initiated with room air in term and late preterm babies and up to 30% oxygen in preterm babies. The use of 100% oxygen during the initial resuscitation has been associated with increased mortality.
- Ventilation corrective steps can be remembered with the mnemonic “MR SOPA.” Once chest movement is achieved, ventilation is continued for 30 seconds, and the heart rate is reassessed.
- MR Mask adjustment
- SO Suction mouth and nose
- Open the mouth, give 5 breaths, and assess chest movement. If no chest movement, continue to the next step.
- P Pressure increase in 5-10 cm increments (maximum 30-40 cm H2O)
- Give 5 breaths after each increment and assess chest movement. If no chest movement at maximum pressure, continue to the next step.
- A Alternative airway
- Confirm insertion. Assess heart rate after 30 seconds of PPV with chest movement.
- An increase in heart rate is the most important indicator that effective ventilation is occurring and that there is an adequate response to resuscitation.
- Specific pulse oximetry goals are determined by minutes of life to guide resuscitation (Table 2).
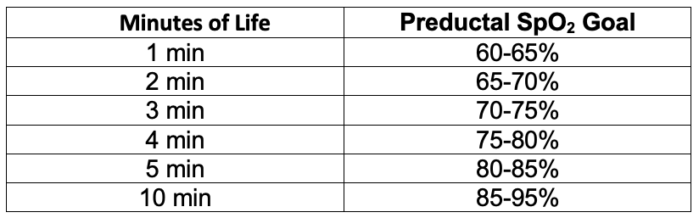
Table 2. Target preductal SpO2 after birth2
- If an alternative airway is needed, a cardiac monitor should be used to continuously assess the infant’s heart rate.
- If the heart rate remains less than 60 beats/minute despite optimizing ventilation, chest compressions should be started. Chest compressions should be coordinated with ventilation in a 3:1 ratio.
- It may be reasonable to use a higher oxygen concentration during chest compressions.
- When performing chest compressions, the 2-thumb-encircling hands technique is associated with improved blood pressure and offers less provider fatigue than the 2-finger technique.
- Prevention of hypothermia should remain an important focus throughout resuscitation efforts.
- Delayed cord clamping is recommended in both term and preterm neonates who do not require resuscitation at birth.
- Routine endotracheal suctioning is no longer recommended in both vigorous and nonvigorous infants with meconium-stained amniotic fluid. It can be beneficial in newborns who have evidence of airway obstruction while receiving PPV.
- When a newborn does not respond to chest compressions and PPV, vascular access should be obtained to deliver volume and epinephrine.
- The umbilical vein is the preferred site of vascular access in newborns to allow for administration of epinephrine.
- If vascular access is unable to be obtained, intraosseous lines should be performed.
- As shown in the NRP algorithm below, when the newborn heart rate remains below 60 beats per minute after 60 seconds of chest compressions and adequate PPV, epinephrine should be administered.
- The preferred method of delivery is intravenous with a dose of 0.01-0.03mg/kg every 3-5 minutes while heart rate is below 60 beats per minute.
- If umbilical venous access is not present, epinephrine can be given endotracheal at a dose of 0.05-0.1 mg/kg every 3-5 minutes; however, IV epinephrine should be given once access is obtained if the response is inadequate.
- If the infant does not respond to epinephrine, volume expansion and other causes of cardiovascular collapse, such as pneumothorax, should be considered.
Neonatal Resuscitation Algorithm
- The NRP algorithm for resuscitation of the newborn is shown in Figure 1.
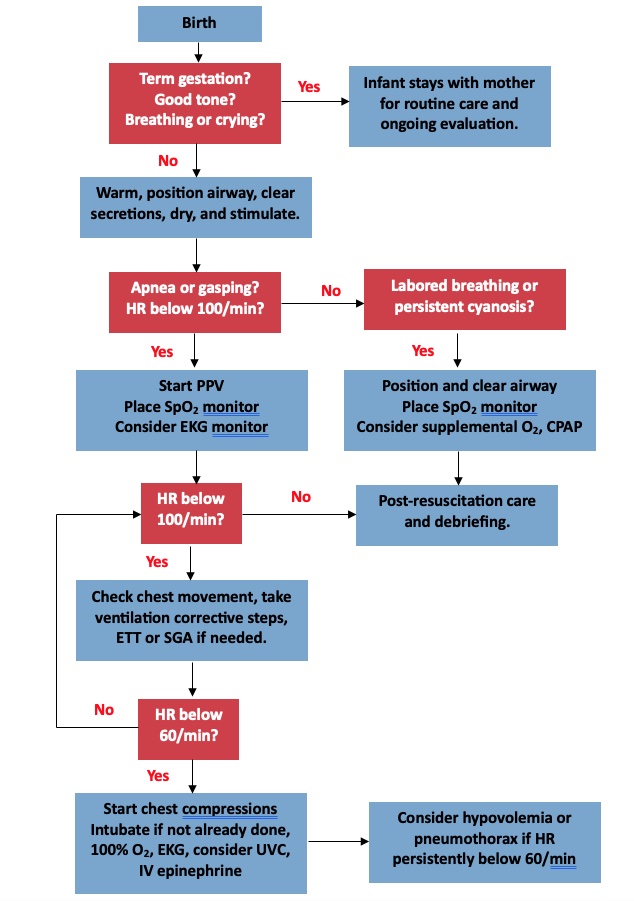
Figure 1. NRP Algorithm for resuscitation of the newborn. Adapted from Aziz K, et al. Part 5: Neonatal resuscitation 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2021. PubMed.
Fetal Cord Blood Gases
- In 1958, it was first reported that umbilical cord blood gases can be analyzed to evaluate for impending fetal hypoxia.4
- Today, umbilical cord blood is recommended in high-risk deliveries by the American College of Obstetricians and Gynecologists (ACOG), given its ability to reflect information about past stresses on the neonate and the current clinical status of the newborn.4
Sampling
- Oxygenated blood travels from the placenta to the fetus via the umbilical vein, circulates through the fetus, and then returns to the placenta via the dual umbilical arteries.5
- Given its larger size, the umbilical vein is easier to sample; however, the umbilical arteries provide more accurate information about the fetal condition and correlate better with outcomes.5
- Venous cord blood provides a more accurate picture of placental metabolism rather than fetal metabolism.
- Venous blood typically has a slightly higher pH and lower PCO2 than umbilical arterial blood for this reason.
- It is important to note that veins are more compressible than arteries, and therefore, venous flow will be more easily decreased during labor or other stressful periods, leading to increased extraction of oxygen by the fetus.5
- This results in more acidotic arterial cord blood, and it is recommended that both venous and arterial blood samples be taken whenever analysis is done.
- The goal of cord blood analysis is to obtain a picture of neonatal acid-base status at the moment of birth when umbilical circulation is arrested by cord-clamping.4
- However, if the umbilical cord remains in continuity with the placenta, placental metabolism will continue and can lead to changes in acid-base status.
- Over a 60-minute period, umbilical arterial and venous pH can fall by 0.2 pH units, with measurements being unreliable as soon as 20 minutes after delivery.5
- For this reason, it is recommended that the umbilical cord undergo double-clamping as early as possible after delivery.4
- Studies have illustrated that pH, PO2, and PCO2 from double-clamped portions of the umbilical cord remain reliable for up to 60 minutes after birth.5
- Lactate levels are undependable as soon as 20 minutes after birth, regardless of cord clamping.
Indications
- Both the ACOG and the AAP recommend that umbilical cord blood be analyzed in all high-risk deliveries when there is suspicion of fetal metabolic abnormalities.5 Examples include category III fetal heart rate tracings and low APGAR scores at birth.
- It is important to note that there is no official global consensus on the exact normal values of cord blood gases. The ranges in Table 3 incorporate generally accepted ranges formed from a compilation of multiple studies.5
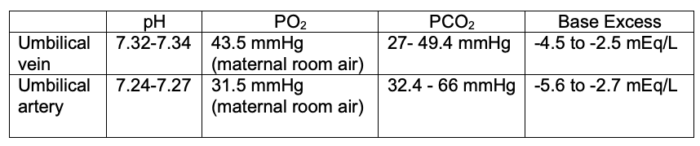
Table 3. Normal ranges of cord blood gases.5
- The “20, 30, 40, 50 rule” is a helpful way to quickly remember normal umbilical cord blood values.
- Umbilical artery PO2➔ 20mmHg
- Umbilical vein PO2➔ 30mmHg
- Umbilical vein PCO2➔ 40mmHg
- Umbilical artery PCO2➔ 50mmHg
Abnormal Findings
- Premature infants often have a higher pH on blood gas analysis and the pH gradually reduces with increased gestational age.4
- A pH less than 7 and a base deficit greater than 12mEq/L have strong correlation with poor neonatal outcomes and are defined as clinically relevant for severe acidemia by the ACOG and AAP.5
- A pH less than 7.10 is often accepted as the statistically defined limit for cord artery acidemia after labor with contractions.
- Even with the mother on supplemental oxygen, the arterial PO2 was never higher than 37.5, so a value greater than this should raise suspicion for air bubbles in the sample.5
- Lactic acid does not cross the placenta and, therefore, provides important and accurate information about the fetal condition. Lactate will increase linearly with advancing gestational age, starting at 34 weeks’ gestation. Typically, a lactate level lower than 10mmol/L at 39 to 40 weeks’ gestation is used as a cutoff for normal.
References
- Gantan EF, Wiedrich L. Neonatal evaluation. Updated 2023. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Link
- Aziz K, Lee C, Henry C, et al. Part 5: Neonatal resuscitation 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2021. PubMed
- Simon LV, Hasmi MF, Bragg BN. APGAR Score. Updated 2023. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Link
- Armstrong L, Stenson BJ. Use of umbilical cord blood gas analysis in the assessment of the newborn. Arch Dis Child Fetal Neonatal Ed. 2007;92(6):430-4. PubMed
- Saneh H, Mendez MD, Srinivasan VN. Cord Blood Gas. Updated 2023. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Link
Other References
- Drzymalski D. Neonatal Resuscitation. OA-SOAP Fellows Webinar Series. 2018. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.