Copy link
Pediatric Difficult Airway
Last updated: 01/25/2023
Key Points
- Children have unique anatomic and physiologic features that may lead to difficult intubation.
- Increased airway reactivity and faster oxygen consumption make children more likely than adults to experience hypoxemia and respiratory complications during airway management.
- If a difficult airway is suspected, it is important to employ apneic oxygenation, have advanced equipment immediately available, and quickly transition to the most experienced provider to limit the overall number of attempts to secure the airway.
Causes of the Difficult Pediatric Airway
- The difficult pediatric airway, whether anticipated or unanticipated, remains an important challenge for anesthesiologists. The consequences of a failed airway can be catastrophic, and children are susceptible to the respiratory and cardiovascular complications associated with a difficult airway due to several unique features.
Anatomical Considerations1
- Larger occiput results in neck flexion and airway obstruction in the neutral position.
- Large tongue and tonsils, compared to the rest of the oral cavity, can cause airway obstruction during mask ventilation.
- More cephalad larynx causes poor alignment of oral, pharyngeal, and laryngeal axes.
- Long and floppy epiglottis can be difficult to lift during laryngoscopy.
- The smaller size of the glottic opening and lower airways make them susceptible to clinically significant obstruction from airway edema resulting from repeated intubation attempts.
Physiological Considerations1
- Infants and young children have a more compliant chest wall that is prone to collapse, leading to atelectasis and decreased functional residual capacity.
- Faster rate of oxygen consumption leads to more rapid arterial desaturation.
- Small children have a more dominant parasympathetic tone that can lead to bradycardia and cardiovascular collapse in response to hypoxemia.
- Increased airway reactivity predisposes children to laryngospasm and bronchospasm.
Associated Syndromes1
Children with certain syndromes, including but not limited to Treacher-Collins, Goldenhar, Apert, Pierre-Robin, and Crouzon syndromes, are known to have difficult airways. A wide range of anatomical abnormalities can be present.
- Maxillary hypoplasia
- Mandibular hypoplasia
- Facial asymmetry
- Large obstructive tongue
- Glottic abnormalities
- Subglottic abnormalities
- Limited mouth opening
- Limited neck mobility
Acquired Conditions can complicate airway management even in healthy children.
- Croup/epiglottitis
- Peritonsillar abscess
- Airway foreign body
- Burns
- Anaphylaxis
- Airway trauma
- Posttonsillectomy hemorrhage
Other Considerations: Education setting where learners are instrumenting the airway.
Incidence and Predictors of Difficult Pediatric Airway
- A small single-center study reported a 6.6% incidence of unexpected difficult bag-mask ventilation (DBMV) in healthy children younger than 8 years. However, this might be an overestimation as the authors defined DBMV as the need for two-person mask ventilation, an oral or nasal airway, the application of continuous positive airway pressure, or the need to increase the oxygen concentration.2
- The APRICOT study, a prospective multicenter observational study that analyzed more than 31,000 anesthetics in children across 261 hospitals in Europe, reported a 0.08% incidence of failed tracheal intubation and a 0.08% incidence of failed supraglottic airway (SGA) insertion.3 Three or more tracheal intubation attempts were necessary in 0.9% of children.
- A secondary analysis of tracheal intubations of the Neonate and Children audit of Anaesthesia pRactice IN Europe (NECTARINE) trial found a high incidence (5.8%) of difficult tracheal intubations (defined as more than two direct laryngoscopy attempts) in children younger than 60 weeks postconceptual age resulting in severe hypoxemia (SpO2 <90% for 60 seconds) in 40% of patients.5
- The Pediatric Difficult Intubation (PeDI) Registry prospectively collected data on 1,018 difficult-to-intubate pediatric patients presenting for anesthesia at 13 pediatric hospitals.4 Of these difficult intubations, 20% were unanticipated.4 More than two tracheal intubation attempts, a weight less than 10kg, short thyromental distance, and three direct laryngoscopy attempts before an indirect technique were associated with an increased risk of complications.4
- The predictors of difficult airway management in children are listed in Table 1.
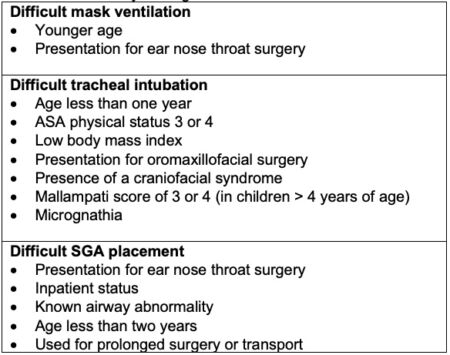
Table 1. Predictors of difficult airway management in children. Adapted from: Burjek NE. The difficult pediatric airway: Predictors, incidence, and complications. In Narasimhan J and Fiadjoe JE, Eds. Management of the Difficult Pediatric Airway. Cambridge UK; Cambridge University Press; 2020: 8-19.
Evaluation of the Pediatric Airway
- A focused airway examination must be performed before every anesthetic. Signs and symptoms of airway obstruction, such as stridor, apneic episodes, cyanosis, dyspnea, and supraclavicular/suprasternal retractions, must be evaluated.
- Evaluation of the pediatric airway can be challenging, particularly in children who are too young to cooperate with the exam or have developmental and cognitive delays that preclude participation. In this group, micrognathia and decreased thyromental distance are the most important physical exam findings that predict difficult tracheal intubation.1
- In healthy children older than four years, the Mallampati index showed a significant correlation with the Cormack-Lehane view. A Mallampati score of 3 or 4 had a 43% positive predictive value for a poor laryngoscopic view.6
Management of the Difficult Pediatric Airway
- The American Society of Anesthesiologists (ASA), Difficult Airway Society, Association of Pediatric Anaesthetists of Great Britain and Ireland (APAGBI), and other individuals have proposed difficult airway algorithms specific to pediatric patients.
- ASA practice guidelines for the management of the difficult airway. PubMed
- Difficult Airway Society and APAGBI Paediatric Difficult Airway Guidelines: PubMed
- A framework for the management of the pediatric airway. PubMed
- The Vortex: a universal high-acuity implementation tool for emergency airway management PubMed.
- If a difficult airway is expected, advanced airway equipment, multiple experienced airway managers, and equipment (endotracheal tubes [ETT], SGAs, oral airways) in multiple sizes should be present prior to induction of anesthesia. In most cases, intravenous access should also be achieved prior to the induction of anesthesia.
- When managing the difficult pediatric airway, the most important goal is to maintain oxygenation and ventilation throughout the procedure. Therefore, end-tidal CO2 and pulse oximetry should be continuously monitored, and apneic oxygenation should be employed when possible. The clinician managing the airway must always be cognizant of the passage of time during each intubation attempt. If the patient begins to desaturate, intubation attempts should be abandoned to re-establish oxygenation and ventilation via mask ventilation or SGA placement.
- Careful attention must be paid to the anesthetic depth during intubation attempts, particularly if neuromuscular blocking drugs are not employed. Laryngospasm is one of the most common respiratory adverse events among the pediatric population and occurs most frequently during a light plane of anesthesia, so it is important to rule it out quickly as a reason for difficult ventilation and oxygenation.
- When assessing the adequacy of ventilation, mask and SGA ventilation should both be considered. SGAs tend to achieve a better seal in children, which, combined with a more compliant chest wall, allows for more effective positive pressure ventilation than in adults. Placement of an SGA in a difficult airway situation may re-establish effective ventilation, allowing the provider to call for help or prepare advanced airway equipment.
- Limiting the overall number of attempts at intubation in the pediatric population should be stressed, as both the APRICOT study and PeDI registry demonstrated a strong association between the number of attempts at instrumenting the airway (whether ETT or SGA) and severe critical respiratory and cardiovascular events.3,4 After each failed intubation attempt, at least one of the following adjustments should be made:
- switch to a more experienced intubating provider;
- make adjustments to the intubation technique (i.e., change patient positioning with a shoulder roll, add a stylet to the ETT, employ apneic oxygenation to prolong the intubating window);
- switch from direct laryngoscopy to an advanced intubation technique (videolaryngoscopy, freehand or SGA-assisted flexible scope intubation);
- switch from one advanced technique to another advanced technique.
- Multiple direct laryngoscope (DL) attempts are associated with complications during difficult pediatric airway management.4 If difficulty is anticipated, the first intubation attempt should be made with an advanced technique. If unanticipated difficulty is encountered, DL should only be repeated one time if an adjustment is made (provider, positioning, laryngoscope blade, etc.) and there is good reason to expect the second DL attempt to be successful. Otherwise, after a failed DL attempt, ventilation should be re-established while advanced equipment is procured and used for the second attempt.
Airway-Related Complications
- In the APRICOT study, 5.2% of all cases involved severe critical events, and 60% of these were respiratory-related. These severe events occurred more frequently in children younger than six months, those younger than 12 months who weighed less than 10 kg, children with micrognathia, cases with repeated instrumentation of the airway, and ICU patients. Laryngospasm and bronchospasm were the most common critical respiratory events, both with an incidence of 1.2%.3
- The PeDI registry data showed that hypoxemia (defined as a 10% decrease from preintubation oxygen saturation for more than 45 seconds) occurred in 9% of difficult intubations and was the most common nonsevere complication, followed by minor airway trauma (4%), laryngospasm (3%), esophageal intubation (3%) and bronchospasm (1%).1 In the PeDI registry data, 2% of the difficult intubations resulted in cardiac arrest, which was the most common severe complication. Hypoxemia preceded all arrests in this cohort.4
References
- Burjek NE. The difficult pediatric airway: Predictors, incidence, and complications. In Narasimhan J and Fiadjoe JE, Eds. Management of the Difficult Pediatric Airway. Cambridge UK; Cambridge University Press; 2020: 8-19.
- Valois-Gomez T, Oofuvong M, Auer G, et al. Incidence of difficult bag-mask ventilation in children: a prospective observational study. Paediatr Anaesth. 2013;23(10): 920-6. PubMed
- Engelhardt T, Virag K, Veyckemans F, et al. Airway management in paediatric anaestheisa in Europe-insights from APRICOT (Anaesthesia Practice in Children Observational Trial): a prospective multicentre observational study in 261 hospitals in Europe. Br J Anaesth. 2018: 121(1): 66-75. PubMed
- Fiadjoe JE, Nishisaki A, Jagannathan N, et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation Registry: A prospective cohort analysis. Lancet Respir Med. 2016;4(1):37-48. PubMed
- Disma N, Virag K, Riva T, et al. Difficult tracheal intubation in neonates and infants. NEonate and Children audiT of Anaesthesia pRactice IN Europe (NECTARINE): a prospective European multicentre observational study. Br J Anaesth. 2021.126(6): 1173-81. PubMed
- Santos AP, Mathias LA, Gozzani JL, et al. Difficult intubation in children: applicability of the Mallampati index. Rev Bras Anestesiol. 2011;61(2): 156-8. PubMed
- Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for management of the difficult airway. Anesthesiology. 2022:136(1): 31-81. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.