Copy link
Fetal Circulation, Transition at Birth, and Persistent Fetal Circulation
Last updated: 06/13/2023
Key Points
- The placenta serves as the organ for gas and nutrient exchange for the fetus.
- Fetal shunts maximize oxygen delivery to the fetal brain and heart.
- At birth, the neonatal circulation transitions; systemic vascular resistance (SVR) increases and pulmonary vascular resistance (PVR) decreases; fetal shunts close, and blood flow to the neonatal lungs increases.
- Persistent fetal circulation results in neonatal hypoxemia and respiratory distress.
Fetal Anatomy
The Placenta
- The placenta is a low-resistance organ that contains 2/3rds of the fetal blood volume and receives 20-33% of fetal cardiac output.1
- It provides the fetus with oxygen and nutrients from the maternal circulation.
- It also transfers fetal carbon dioxide and waste products from the fetal to the maternal circulation.
Fetal Blood Flow
- Oxygenated blood from the placenta travels via the umbilical vein into the fetal liver and then into the inferior vena cava (IVC) via the ductus venosus (Figure 1).
- Blood travels to the right atrium, where it mixes with systemic blood.
- Oxygenated blood is then preferentially shunted across the foramen ovale into the left atrium and into the systemic circulation; deoxygenated blood from the superior vena cava (SVC) continues to the right ventricle and pulmonary circulation.
- Blood flow to the fetal lungs is additionally limited by the ductus arteriosus, which shunts blood from the pulmonary to systemic circulation.
- Blood returns to the placenta via the paired umbilical arteries.
- The fetal circulation is described as a parallel circuit where both ventricles provide systemic blood flow and several shunts allow the mixing of oxygenated and deoxygenated blood.
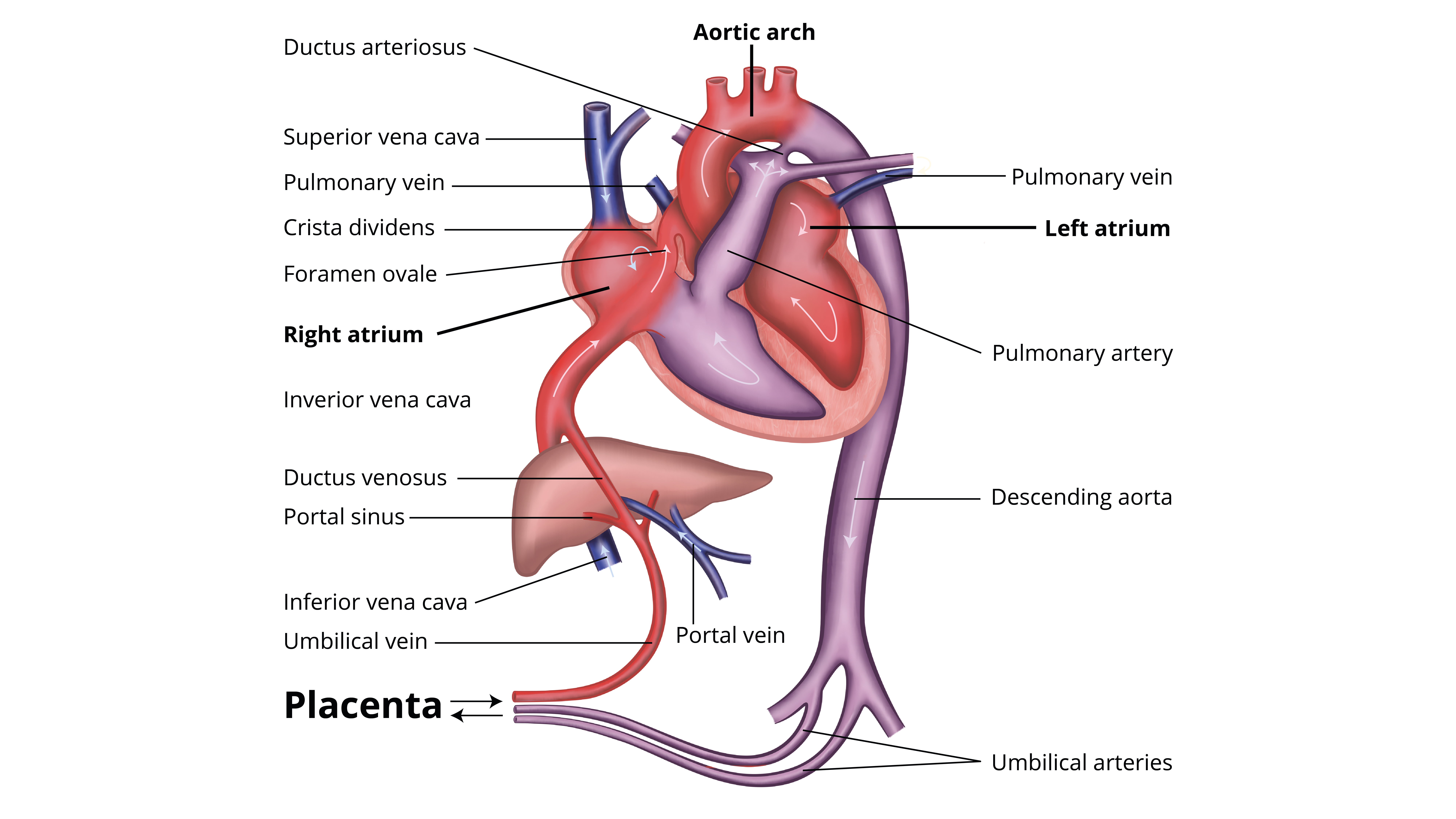
Figure 1. Schematic of fetal circulation. Note the coloring of oxygen-rich (red), oxygen-poor (blue) and mixed (purple) blood.
Fetal Shunts
- Three fetal shunts optimize oxygen delivery to the fetal brain and heart.
- Ductus venosus is in the fetal liver. It bypasses the portal circulation and directs oxygenated blood to the heart.
- Foramen ovale is located across the fetal atrial septum. It is anatomically positioned to direct oxygenated blood to the heart and brain.
- Ductus arteriosus is located between the pulmonary artery and aorta. It directs blood flow away from the fetal lungs, which are fluid filled and have high vascular resistance due to low oxygen tension.
Fetal Hemoglobin/Oxygen Transport
Fetal Hemoglobin
- Fetal hemoglobin (HbF) consists of two alpha and two gamma subunits, while adult hemoglobin (HbA) has two alpha and two beta subunits.
- HbF has a higher affinity for oxygen compared to Hgb A, which ensures oxygen uptake from the maternal circulation.
- P50, the partial pressure at which 50% of the oxygen molecules are saturated with oxygen of HbF is 19 mmHg, compared to 27 mmHg for HbA.
- HbF also has decreased affinity to 2,3-bisphosphoglycerate compared to HbA, which also favors oxygen transfer.
- After 20 weeks of gestation, HbF is gradually replaced by HbA, and it reaches adult levels by approximately 6 months of age.2
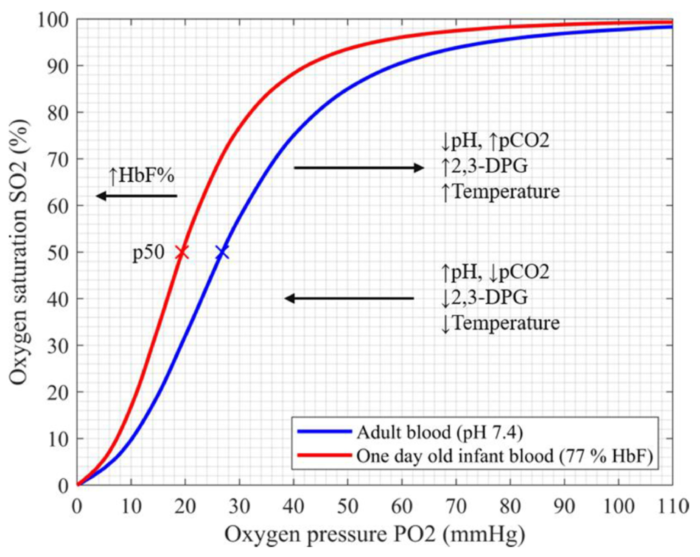
Figure 2. Oxyhemoglobin desaturation curves for fetal (red line) and adult (blue line) hemoglobin. The p50, or partial pressure at which 50% of the hemoglobin molecules are saturated with oxygen is 19 mmHg for HbF compared to 27 mmHg for HbA. This results in fetal oxygen uptake from maternal blood. Source: Pritišanac E, et al. Accuracy of pulse oximetry in the presence of fetal hemoglobin—A systematic review. Children. 2021; 8(5):361.2 CC BY 4.0.
Fetal Oxygenation
- The intrauterine oxygen tension is low compared to extrauterine life. The highest fetal oxygen levels are found in the umbilical vein (umbilical venous PaO2 = 55 mmHg) and the lowest oxygen levels are found in the umbilical arteries (umbilical arterial PaO2 = 15-25 mmHg).3
- Fetal tissue oxygenation is maintained by:
- Fetal hemoglobin
- Decreased fetal oxygen consumption
- Fetal shunts, which optimize oxygen delivery
- A higher fetal hematocrit (approximately 55% in utero)
Transition to Neonatal Circulation
At birth, the circulation transitions from a fetal to neonatal circulation (Figure 3):
- With the infant’s first breath, the following occurs:
- Lung expansion→establishes functional residual capacity and promotes surfactant release
- Reduction in lung fluid volume→due to negative hydrostatic pressure and epithelial changes
- Lung expansion drops PVR and pulmonary artery (PA) pressures.
- Placental clamping increases SVR.
- Foramen ovale closes with increased blood flow/pressure in the left atrium when left atrial pressures exceed right atrial pressures.
- Ductus arteriosus reverses from R→L to L→R due to increased SVR and decreased PVR.
- Over time, higher oxygen tensions lead to epithelization of the ductus.
- Targets for preductal oxygen saturation during neonatal resuscitation include4
- 1 minute – 60 to 65 percent
- 2 minutes – 65 to 70 percent
- 3 minutes – 70 to 75 percent
- 4 minutes – 75 to 80 percent
- 5 minutes – 80 to 85 percent
- 10 minutes – 85 to 95 percent
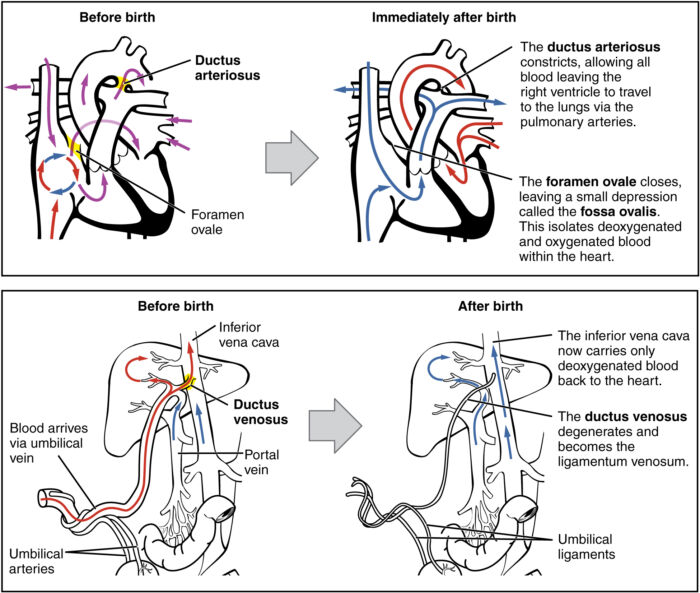
Figure 3. Changes in the neonatal circulation seen following birth. Note the coloring of oxygen-rich (red), oxygen-poor (blue) and mixed (purple) blood. Source: OpenStax College Wikimedia CC-BY-3.0. Link.
Persistent Fetal Circulation
Approximately 10% of neonates have impaired transition to neonatal circulation and require some intervention, and less than 1% of newborns require extensive resuscitation at birth.
Etiology
- Absent or minimal respiratory effort: birth asphyxia, maternal anesthesia/opiates, congenital neuromuscular disorders
- Mechanical airway obstruction: meconium aspiration, congenital airway anomalies, such as micro/retrognathia, laryngeal webs, etc.
- Lung disorders: prematurity, congenital diaphragmatic hernia, pneumothorax, delayed pulmonary fluid clearance, group B Streptococcal pneumonia
- Congenital heart disease
- Preterm infants
Consequences
- Persistent pulmonary hypertension of the newborn occurs when the PVR remains elevated after birth. This results in persistent R→L shunting across the foramen ovale and ductus arteriosus.
- Preductal oxygen saturation is often 10% higher than post ductal oxygen saturation.
- This can result in severe hypoxemia and hypercapnia.
Treatment
- The neonatal resuscitation program (NRP) algorithm should be followed.
- Endotracheal intubation should be performed.
- Controlled ventilation should be used if there is minimal or no respiratory effort.
- The FiO2 should be increased to target expected oxygen saturation.
- The underlying cause should be treated when possible.
References
- Kiserud T, Ebbing C, Kessler J, et al. Fetal cardiac output, distribution to the placenta and impact of placental compromise. Ultrasound Obstet Gynecol. 2006 Aug;28(2):126-36. PubMed
- Pritišanac E, Urlesberger B, Schwaberger B, et al. Accuracy of pulse oximetry in the presence of fetal hemoglobin—A systematic review. Children. 2021; 8(5):361. PubMed
- Soothill PW, Nicolaides KH, Rodeck CH, et al. Blood gases and acid-base status of the human second-trimester fetus. Obstet Gynecol. 1986;68(2):173-6. PubMed
- Noori S, Wlodaver A, Gottipati V, et al. Transitional changes in cardiac and cerebral hemodynamics in term neonates at birth. J Pediatr. 2012;160(6):943-8. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.