Copy link
Polymorphic VT: Rx
Last updated: 03/06/2015
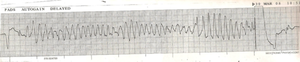
Polymorphic Ventricular Tachycardia (Torsade de Pointes) is a ventricular arrhythmia characterized electrographically by a wide complex tachycardia that appears to twist around a single point, as the amplitude of the waves enlarge and shrink. Torsades usually occurs in a “pause dependent” fashion. There is a run of tachycardia, or an ectopic beat, and then a post-ectopic pause. The QT interval of the next supraventricular beat is substantially prolonged and thus the subsequent depolarization (R wave) occurs during the relative refractory period of repolarization (R on T phenomenon) and sets up re-entrant circuits, leading to Torsades.
A prolonged QT interval is classically thought to be the most important risk factor for Torsades (although the short QT variant was described in 1994.) A QT interval above 470msec for men and 480msec for women is defined as prolonged, although the interval needs to be corrected for heart rate since it will lengthen with bradycardia. There is a congenital long QT syndrome, which is a disorder of either cardiac calcium or potassium channels (IKr.) Acquired long QT is mainly associated with specific drugs that affect these channels such as typical anti-psychotics, anti-fungals, certain anti-emetics, some anesthetics and anti-arrhythmics. Hypokalemia or hypomagnesemia are often associated with drug-induced Torsades. Women generally have a longer QT interval than men.
Prevention of the arrhythmia by maintaining a normal QT in those without genetic predisposition is the best management. However, once Torsades starts, it is usually self-limiting or can devolve into ventricular fibrillation. At this point, any offending drugs should be discontinued. There are two general approaches to treatment: 1) Shorten the action potential or 2) Inhibit triggered activity. Overdrive pacing either transcutaneously or transvenously to a heart rate above 90bpm will effectively shorten the action potential. Isoproterenol and dobutamine have also been used for this. IV magnesium and beta blockers act by inhibiting triggered activity, but they do not shorten the QT interval. If there is hemodynamic compromise, the patient should be asynchronously cardioverted and ACLS should be initiated.
Magnesium sulfate is the treatment of choice to prevent recurrence. Patients should receive an initial bolus of 30 mg/kg intravenously, followed by an infusion of 2– 4 mg/min. The bolus may be repeated after 15 min.
References
- Susan J Kies, Christina M Pabelick, Heather A Hurley, Roger D White, Michael J Ackerman Anesthesia for patients with congenital long QT syndrome. Anesthesiology: 2005, 102(1);204-10 PubMed Link
- D M Roden A practical approach to torsade de pointes. Clin Cardiol: 1997, 20(3);285-90 PubMed Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.