Copy link
Hypokalemia
Last updated: 09/20/2023
Key Points
- Hypokalemia is defined as the reduction of serum potassium levels below normal (usually less than 3.5 mEq/L). However, the definition may vary depending on institutional laboratory values.1
- Elective surgeries should be postponed in patients with serum potassium levels less than 3.0 mEq/L.
- The primary treatment of hypokalemia is cardiac stabilization with return of normal neuromuscular function, and potassium replacement is the mainstay of therapy.
Etiology
Hypokalemia can occur because of a transcellular shift in potassium or a decrease in total body potassium stores.1-3
Transcellular Shifts in Potassium
- Beta-agonist therapy can produce a mild decrease in potassium (less than 0.5 mEq/L) by stimulating beta-2 receptors in the skeletal muscle.1
- Alkalosis can promote intracellular shift of potassium in exchange for hydrogen ions via the H+/K+ exchange pump.1
- Hypothermia can cause a transient drop in potassium that resolves with rewarming.1
- Insulin use can drive potassium intracellularly via glucose transport mechanisms, and its effects last 1-2 hours.1
- Lithium overdose as well as B12 therapy can also cause hypokalemia.3
Decrease in Total Body Potassium
- Inadequate intake secondary to alcoholism, anorexia, malnutrition, etc.3
- Excessive gastrointestinal losses from vomiting, diarrhea, fistulas, etc.3 The total potassium in gastric secretions is relatively low (10-15mEq/L); however, the volume loss and alkalosis promotes increased renal losses of potassium.1
- Excessive renal losses secondary to mineralocorticoid/glucocorticoid excesses, lop or thiazide diuretics, osmotic substances, hypomagnesemia, renal tubular acidosis, etc.3
Typical Situations
- Hypokalemia can occur postoperatively following cardiac surgery.5 This can be secondary to cardiopulmonary bypass as well as the administration of insulin and glucose which can cause a shift from extracellular to intracellular potassium.
- Chronic renal insufficiency patients can tolerate chronic elevations in potassium much better than acute changes because equilibration of serum and intracellular stores of potassium takes place over time, returning the resting membrane potential of excitable cells to nearly normal.4 Chronic renal insufficiency patients are no more susceptible to the hyperkalemic effects of succinylcholine than those with normal functioning kidneys.4
- Hyperventilation due to alkalosis causes a promotion of intracellular K+ in exchange for hydrogen ions via a membrane H+/K+ pump.1 In general, alkalosis causes a variable and unpredictable change in potassium.
- Beta adrenergic stimulation, such as the administration of albuterol and dobutamine5
- Patients with hyperaldosteronism which can cause hypokalemia by increasing renal potassium excretion
- Patients receiving diuretics (thiazides, furosemide), secondary to increased aldosterone secretion, alkalemia, and increased renal tubular flow.2
- Renal tubular damage due to nephrotoxins, such as aminoglycosides or amphotericin B2
Prevention
- Hypokalemia alone is not a risk for arrhythmias. However, it can add to the risk of arrhythmias from other patient comorbidities. No clear guidelines for hypokalemia have been established. A potassium value of less than 3.5mEq/L in cardiac surgical patients has been shown to have an increased incidence of perioperative dysrhythmias.2
- It is accepted that elective surgery should be postponed if the patient’s serum potassium is below 3.0 mEq/L and potassium supplementation should be administered prior to the anesthetic.2
- After potassium supplementation, the patient’s serum potassium levels should be rechecked prior to administering the anesthetic. Patients should be assessed for any risk factors for hypokalemia, such as chronic diuretic use, renal dysfunction, or gastrointestinal losses.
- Conditions that cause hypokalemia such as hyperventilation, metabolic alkalosis, and beta-adrenergic stimulation should be avoided.5
- Hypomagnesemia is a known cause of hypokalemia and is present in up to 40% of hypokalemic patients.1 It is thought to impair the thick ascending limb sodium reabsorption, causing increased sodium distal delivery and potassium loss via the principal cells.3
Diagnosis & Management
- Hypokalemia is typically diagnosed with a serum potassium level measurement. It is assumed that hypokalemia can cause an increase in morbidity and mortality; however, there is little evidence to support this.3 In fact, the majority of patients with hypokalemia are asymptomatic.1
- The symptoms of hypokalemia are primarily neuromuscular and cardiovascular in nature. Patients with severe hypokalemia can present with significant weakness, and as acute hypokalemia progresses, paralysis can ensue.2
- As a general rule, 1mEq/L decrease in the plasma potassium is equivalent to 200-300mEq total potassium deficit.2
- Cardiac manifestations of hypokalemia can be present in up to 50% of cases.1 ECG findings classically seen are prominent U waves, flattening of T waves, and prolongation of the QT interval (Figure 1).
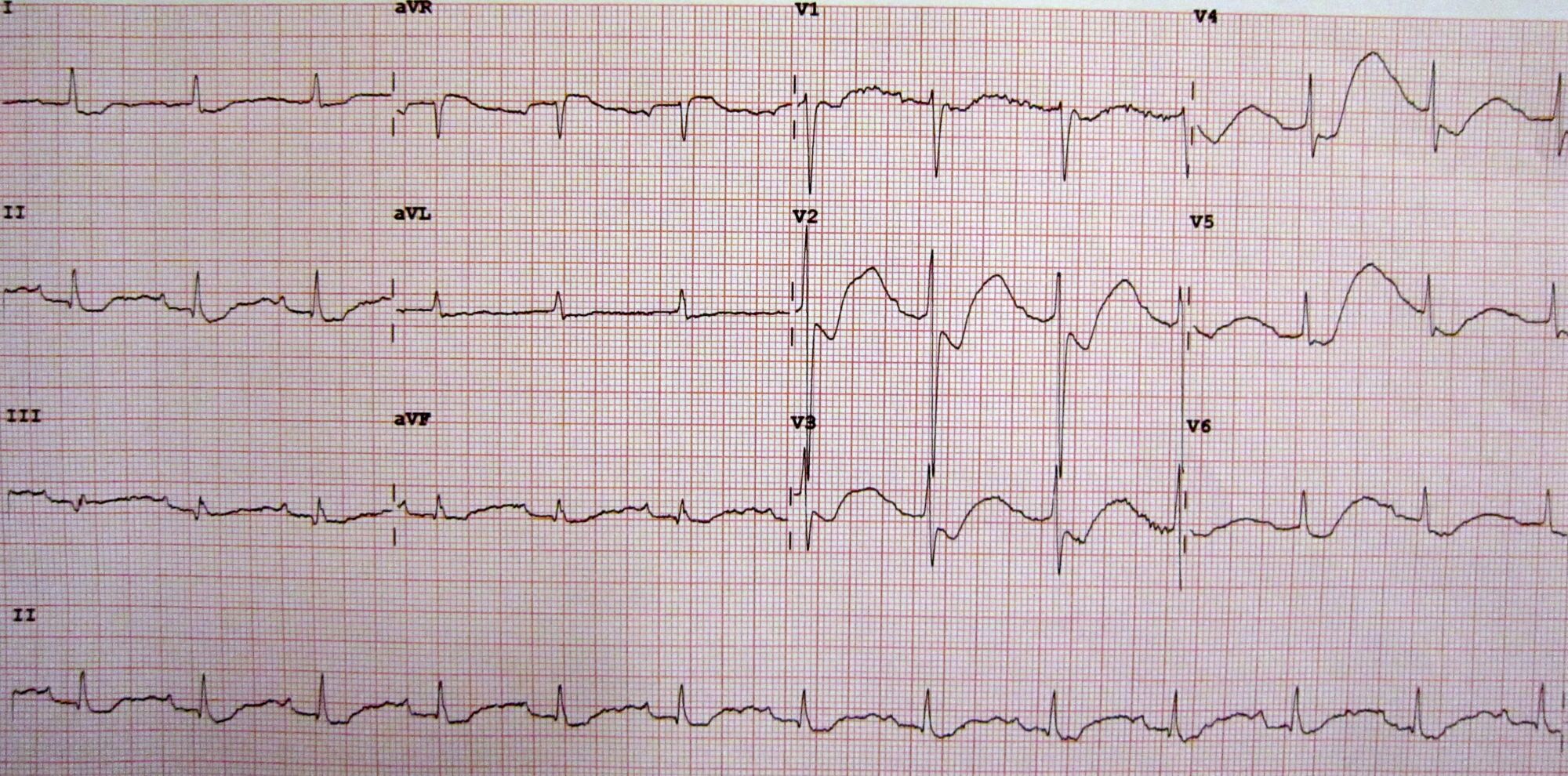
Figure 1. An electrocardiogram (ECG) of a patient with a potassium level of 1.1 showing the classical ECG changes of ST segment depression, inverted T waves, large U waves, and a slightly prolonged PR interval. Source: Wikimedia Commons. James Heilman, MD, CC BY-SA 3.0 Link.
- Elective surgery should be postponed for potassium levels below 3.0 mEq/L and oral potassium replacement (typically 20 to 80mEq/day) should be prescribed.4
- For urgent or emergent surgery in patients with potassium levels less than 3.0 mEq/L, intravenous potassium replacement may be necessary. The standard rate of replacement of potassium is 20 mEq/hr, but 40mEq/hr may be necessary in cases of extreme hypokalemia (less than 1.5mEq/L).1
- With extreme cases of hypokalemia, the response to treatment may be slow. This is due to the fact that a total body deficit of 200-400 mEq of potassium is needed to drop the potassium by 1 mEq, however it only takes 1-200 mEq of excess potassium to increase the potassium 1 mEq. Thus, a change in total body potassium is twice as great with deficit compared to excess.1 This can be visualized in figure 2 below:
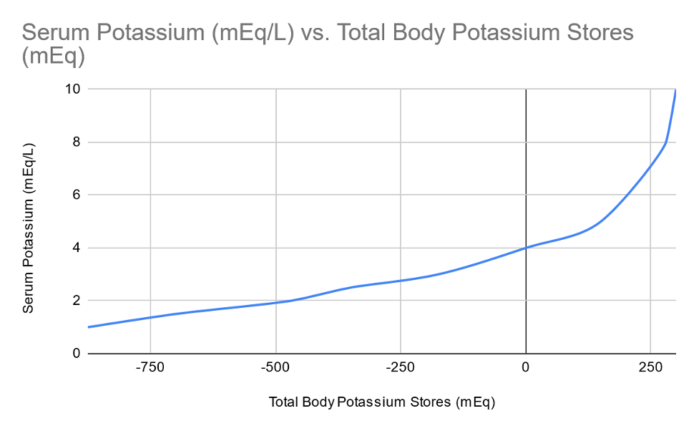
Figure 2. Relationship between total body potassium and the serum potassium concentration. Redrawn from data in Reference 6.
- If hypokalemia is refractory to treatment, hypomagnesemia may be considered, as potassium replacement therapy is often ineffective in the presence of low magnesium.
References
- Marino PL, Galvagno SM Jr. Potassium. In: Marino’s The Little ICU book, 2nd Edition. Philadelphia, PA. Wolters Kluwer Health; 2017: 367-371.
- Prough DS, Funston JS, Saad AF, et al. Fluids, electrolytes, and acid base physiology. In: Barash PG (ed). Clinical Anesthesia, 8th Edition. Philadelphia, PA. Wolters Kluwer Health. 2017: 1051-6.
- Edwards MR, Grocott MPW. Perioperative fluid and electrolyte therapy. In: Miller R (ed). Miller's Anesthesia. 9th edition. Philadelphia, PA; Elsevier/Saunders; 2019: 1480-1523.
- Brull SJ, Meistelman C. Pharmacology of neuromuscular blocking drugs. In: Miller RD (ed). Miller's Anesthesia. 9th edition. Philadelphia, PA; Elsevier/Saunders; 2019: 792-831.
- Botz GH. Metabolic events. In: Gaba DM, Burden AR, Howard SK, et al. Crisis Management in Anesthesiology. 2nd Edition. Philadelphia, PA. Elsevier/Saunders; 2015: 214-7.
- Brown RS. Extrarenal potassium homeostasis. Kidney Int. 1986; 30:116–127. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.