Copy link
Amniotic Fluid Embolism
Last updated: 09/27/2023
Key Points
- Amniotic fluid embolism (AFE) is a rare but potentially life-threatening complication of pregnancy.
- AFE classically presents as acute respiratory distress, hypotension/hemodynamic instability, and coagulopathy.
- AFE occurs most often during labor and in the immediate postpartum period.
- Early recognition and aggressive resuscitation are crucial to improve maternal and fetal outcomes.
Introduction
- Amniotic fluid embolism is a potentially catastrophic obstetric complication.
- The true incidence of AFE is unknown because of significant variability in the diagnostic criteria and reporting methodology used.1
- The mortality rate varies widely depending on the source, but may be as high as 60%.1
- There is no definitive test used to diagnose AFE, and the signs and symptoms are nonspecific.
Etiology
• Emboli of fetal material alone are insufficient to trigger an AFE.
• The presence of fetal antigens leads to a cascade of inappropriately released inflammatory mediators (thromboxane, leukotrienes, prostaglandins, endothelins)1-3 (Figure 1).
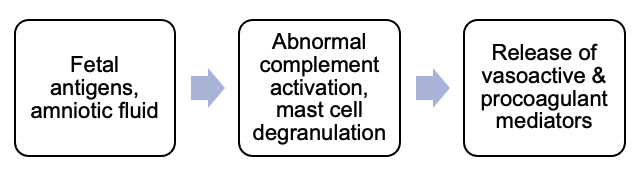
Figure 1. Pathophysiology of AFE
- The previously used term “anaphylactoid syndrome of pregnancy” may then be inaccurate as the cascade likely causes mast cell degranulation, as opposed to the other way around.2
- Risk factors for AFE are listed in Table 1.
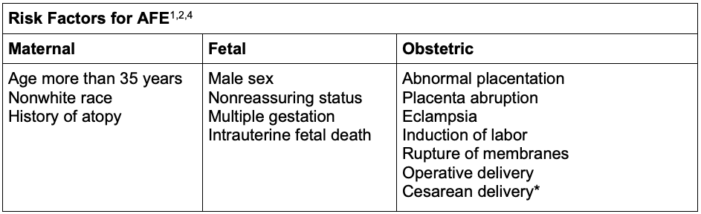
Table 1. Risk factors for AFE
*Cesarean delivery may be a consequence, as opposed to a cause, because of the associated nonreassuring fetal heart rate tracing seen with AFE.
Abbreviation: AFE, Amniotic fluid embolism
Diagnosis
- AFE is a clinical diagnosis and there is no definitive test used to diagnose AFE.
- Commonly used clinical criteria have been established including:
- Acute hypotension, cardiac arrest/collapse
- Acute respiratory compromise
- Coagulopathy
- Onset during labor, cesarean delivery, dilation and evacuation or within 30 minutes postpartum
- Absence of another clear cause or diagnosis
- Of note, AFE may also occur up to 48 hours postdelivery and after abdominal trauma, first trimester abortion, in the second trimester, and during an amnioinfusion.2
- The differential diagnosis is broad as many of the signs and symptoms are nonspecific (Table 2).
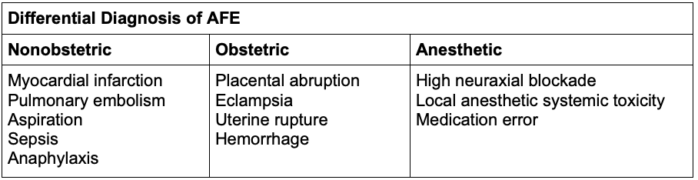
Table 2. Differential diagnosis of AFE
Abbreviation: AFE, Amniotic fluid embolism
- Common signs and symptoms of AFE are listed in Table 3.
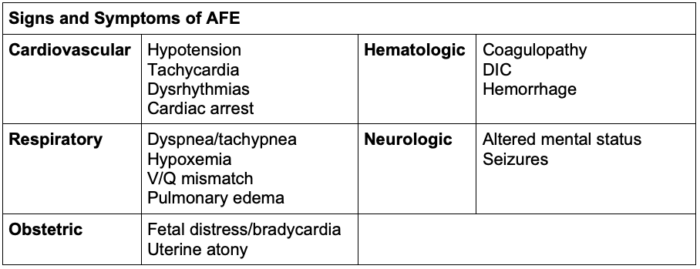
Table 3. Signs and symptoms of AFE
Abbreviation: AFE, Amniotic fluid embolism; DIC, disseminated intravascular coagulation; V/Q, ventilation/perfusion
- There is a biphasic cardiovascular response during AFE.2
1. Within the first 30 minutes (Figure 2):
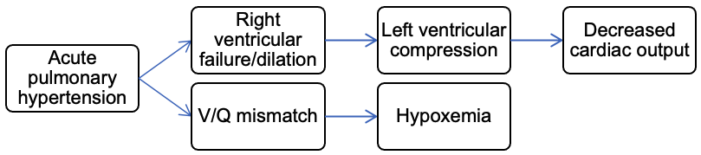
Figure 2. Early clinical presentation of AFE
2. If the patient survives the first phase, left ventricular failure and pulmonary edema may result (Figure 3).
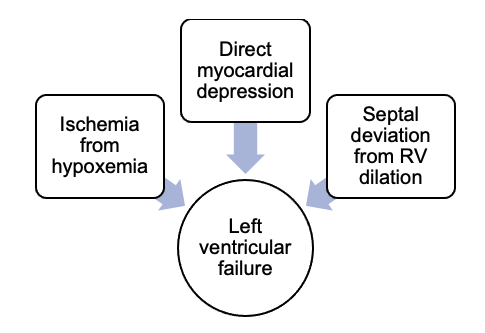
Figure 3. Pathophysiology of left ventricular failure in AFE
- With survival to the second phase, patients also concomitantly experience disseminated intravascular coagulation (DIC) and hemorrhage.
- However, AFE may present atypically with DIC and hemorrhage without preceding cardiovascular collapse.2
Management
- The treatment of AFE is largely supportive.1
- Aggressive clinical management should focus on cardiovascular support, treatment of hypoxemia, and management of hemorrhage and coagulation abnormalities for the optimization of maternal and fetal well-being.
- Patients often present with cardiac arrest (Table 4).
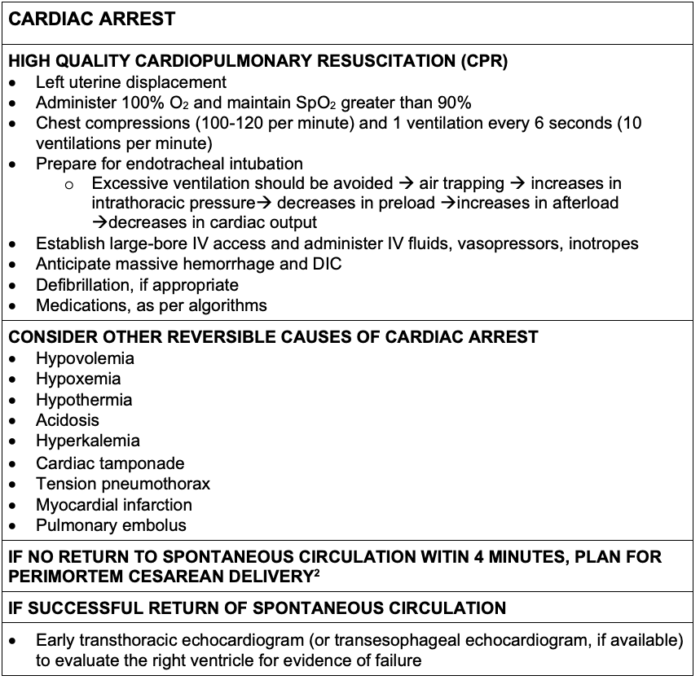
Table 4. Management of cardiac arrest during pregnancy
Abbreviation: DIC, disseminated intravascular coagulation
- If there is evidence or high suspicion of acute RV failure, management includes:
- Vasopressors (i.e., norepinephrine)
- Inotropes (i.e., milrinone or dobutamine)
- Pulmonary vasodilators (i.e., inhaled nitric oxide or epoprostenol)
- Avoidance of excessive fluid administration
- If the patient remains hemodynamically unstable or requires prolonged CPR despite interventions, consider extracorporeal membrane oxygenation (ECMO).3
Disseminated Intravascular Coagulation
- Amniotic fluid contains tissue factor, which binds to factor VII and activates the coagulation cascade.3
- The coagulopathy is related to both consumption and hyperfibrinolysis.2,3
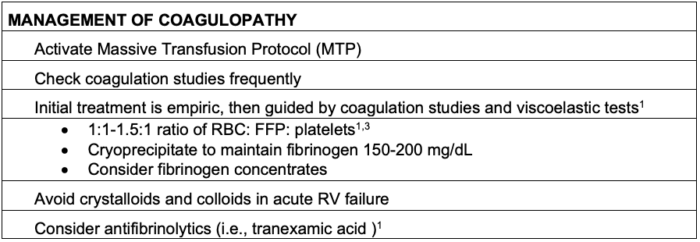
Table 5. Management of coagulopathy from AFE
Abbreviations: RBC, red blood cells; FFP, fresh frozen plasma; RV, right ventricular
References
- Sultan P, Seligman K, Carvalho B. Amniotic fluid embolism: update and review. Curr Opin Anaesthesiol. 2016;29(3):288-96. PubMed
- Toledo P. Embolic disorders. In: Chestnut D, Wong CA, Tsen LC, Ngan Kee W, Beilin Y, Mhyre JM, Bateman B, eds. Chestnut’s Obstetric Anesthesia: Principles and Practice. 6th ed. Philadelphia: Elsevier; 2020: 943-48.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222(1):48-52. PubMed
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the Unites States International Registry. Am J Obstet Gynecol MFM. 2020;2(2):100083. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.