Copy link
Obstructive Sleep Apnea: Preoperative Screening Tools and Testing
Last updated: 11/10/2023
Key Points
- Polysomnography remains the gold standard for the diagnosis of obstructive sleep apnea (OSA), but its use is limited due to time and resource constraints.
- Routinely deferring surgery for polysomnographic confirmation of OSA is not recommended.
- Screening questionnaires like the STOP-Bang are commonly used in addition to clinical findings in the perioperative period.
Preoperative Assessment
- Polysomnography is the gold standard for the diagnosis of OSA. However, it is unsuitable for routine preoperative risk assessment due to limitations of time, resources, and logistics.
- OSA is classified as mild, moderate, and severe based on the apnea-hypopnea index (AHI) during an overnight polysomnography. In adults, the AHI cutoffs for defining the severity of OSA are as follows.
- Mild OSA: 5 to less than 15 events/hour
- Moderate OSA: 15-30 events/hour
- Severe OSA: More than 30 events/hour
- Patient interviews, previous health evaluations, physical examinations, and screening questionnaires are commonly used in the perioperative period.
- Identifying patients at high risk for OSA helps in risk stratification.
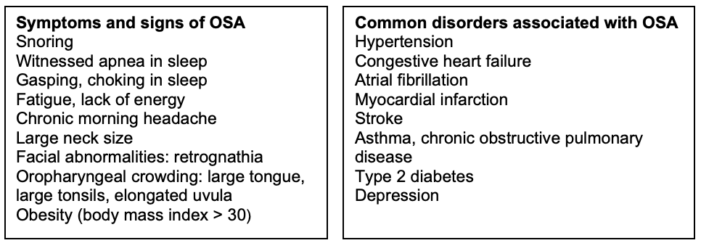
Table 1. Clinical presentation and common disorders associated with OSA
Screening Questionnaires
• Multiple screening questionnaires have been validated for preanesthetic risk stratification.
• Commonly used are the STOP-Bang questionnaire, the Perioperative Sleep Apnea Prediction score (P-SAP), and the Berlin questionnaire.
• The STOP-Bang questionnaire and Berlin questionnaire have been found to be sensitive to screen presurgical patients for OSA.1
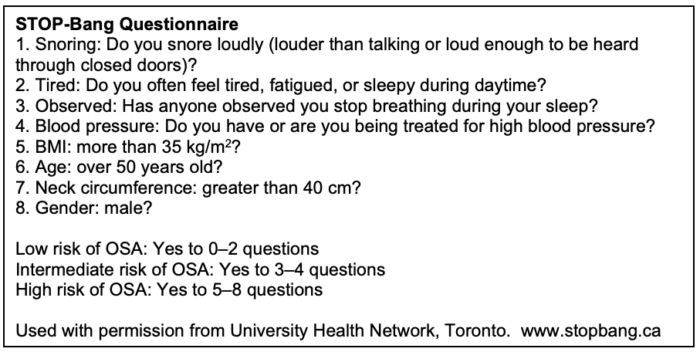
Table 2. STOP-Bang Questionnaire. Used with permission from University Health Network, Toronto. Link.
Preoperative Screening Considerations
The Society of Anesthesia and Sleep Medicine guidelines for preoperative screening and assessment of adult patients with OSA includes the following recommendations.2
Recommendations for Screening to Identify Patients with Suspected OSA
- Patients with a diagnosis of OSA should be considered to be at an increased risk for perioperative complications. (Level of Evidence (LOE) Moderate, Grade of Recommendation (GOR) Strong)
- Adult patients at risk for OSA should be identified before surgery. (LOE Low, GOR Weak)
- Screening tools help risk stratify patients with OSA and should be included in the standard preanesthetic evaluation. (LOE Moderate, GOR Strong)
- There is insufficient evidence to delay/cancel surgery to obtain a formal diagnosis of OSA, unless there is evidence of significant associated systemic disease or problems with ventilation/ gas exchange. (LOE Low, GOR Weak)
Recommendations for Surgical Patients with OSA Who Are Adherent to Positive Airway Pressure (PAP) Therapy
- The patient, surgeon, anesthesiologist, and the care team should be aware before the procedure that the patient carries a diagnosis of OSA, which may increase postoperative morbidity. (LOE Low, GOR Strong)
- The results of a previous sleep study and positive airway pressure (PAP) setting, if available, should be obtained before the surgery. (LOE Low, GOR Weak)
- Facilities should consider having PAP equipment available for perioperative use or the patient should be instructed to bring in their own PAP equipment. (LOE Low, GOR Strong)
- Patients should continue to wear their PAP device at appropriate times during their stay in the hospital, both preoperatively and postoperatively. (LOE Moderate, GOR Strong)
Recommendations for Surgical Patients with OSA Who Decline or Are Poorly Adherent to PAP Therapy
In addition to the recommendations above, the following is recommended.
- Additional evaluation for preoperative cardiopulmonary optimization should be considered in patients with diagnosed, partially treated/untreated, and suspected OSA where there is indication of an associated significant or uncontrolled systemic disease or additional problems with ventilation or gas exchange such as:
- hypoventilation syndromes;
- severe pulmonary hypertension; and
- resting hypoxemia in the absence of other cardiopulmonary disease. (LOE Low, GOR Weak)
- Untreated OSA patients with optimized comorbid conditions may proceed to surgery, provided strategies for mitigation of postoperative complications are implemented. (LOE Low, GOR Weak)
- The risks and benefits of a decision to proceed with/delay surgery should involve consultation and discussion with the surgeon and patient. (LOE Low, GOR Weak)
Recommendations for Surgical Patients Who Have a High Probability of OSA
- The patient and the health care team should be aware that a high probability of OSA may increase postoperative morbidity. (LOE Low, GOR Strong)
- Continued use of PAP therapy at previously prescribed settings is recommended during sleep while hospitalized, both preoperatively and postoperatively. (LOE Moderate, GOR Strong)
- Patients should be advised to notify their primary medical provider that they were found to
have a high probability of having OSA, thus allowing for appropriate referral for further evaluation (LOE Low, GOR Strong).
Recommendations for Preoperative Management of OSA4
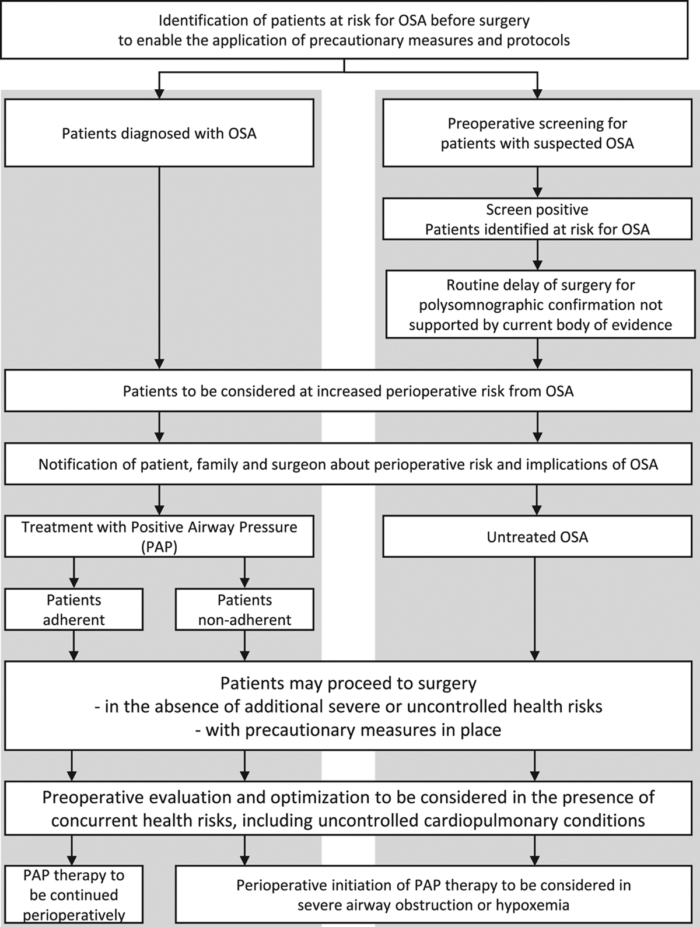
Figure 1. Recommendations for the preoperative management of OSA from the Society of Anesthesia and Sleep Medicine and the American Society of Anesthesiologists Task Force on perioperative management of patients with OSA. Used with permission from Cozowicz C, Memtsoudis SG. Perioperative management of the patient with obstructive sleep apnea: A narrative review. Anesth Analg. 2021.3
References
- Nagappa M, Liao P, Wong J, et al. Validation of the STOP-Bang questionnaire as a screening tool for obstructive sleep apnea among different populations: A systematic review and meta-Analysis. PLoS One. 2015; 10(12): e0143697. PubMed
- Chung F, Memtsoudis SG, Ramachandran SK, et al. Society of Anesthesia and Sleep Medicine guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg. 2016;123(2):452-73. PubMed
- Cozowicz C, Memtsoudis SG. Perioperative management of the patient with obstructive sleep apnea: A narrative review. Anesth Analg. 2021;132(5):1231-43. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.